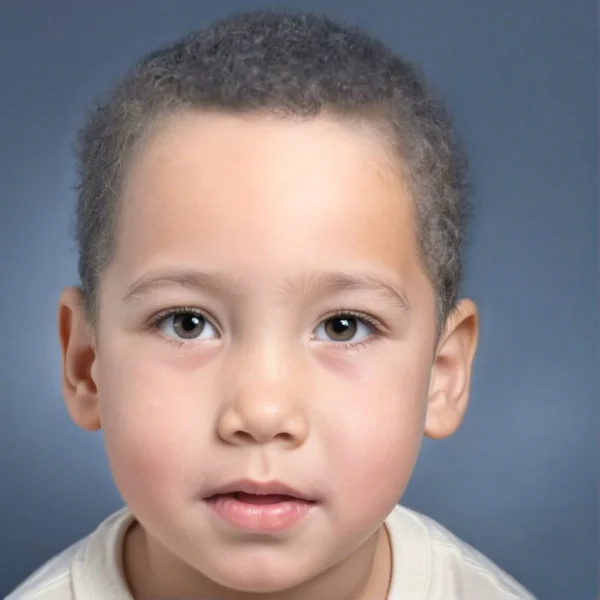
Poliosis is a condition characterized by the loss or absence of melanin in hair follicles It manifests as white or gray patches of hair on the scalp, eyebrows, eyelashes, or other hair-bearing regions. This phenomenon occurs when melanocytes, the cells responsible for producing melanin (the pigment that gives hair its color), are either absent or malfunctioning in specific regions of the body. Although gray hair is associated with the normal process of aging, when it appears in younger individuals or in localized areas, it can be a sign of underlying genetic, autoimmune, or neurological conditions. In this article, we will explore the underlying mechanisms of poliosis, its associations with various diseases, and the clinical implications.
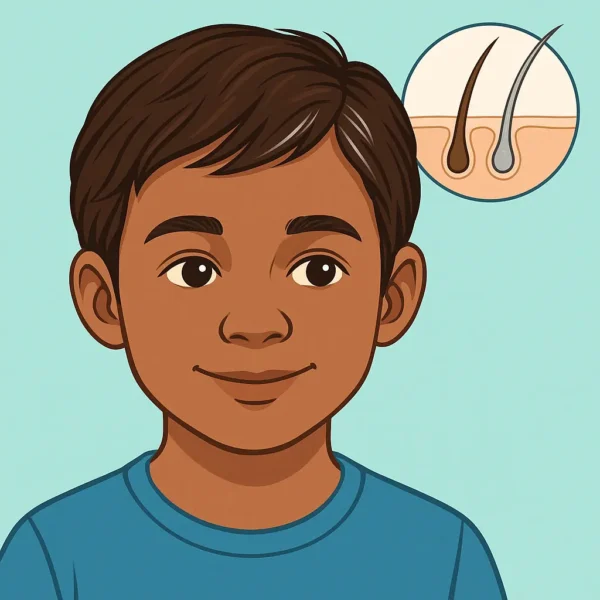
Mechanisms of Melanin Production and Loss in Hair: To understand poliosis, it is useful to understand the normal process of melanin production and its role in hair pigmentation. Melanocyte cells, located in the hair follicle’s bulb, synthesize melanin through a process regulated by several enzymes, including tyrosinase. Melanin is classified into two types: eumelanin, responsible for black and brown hues, and pheomelanin, responsible for red and yellow tones. The balance and distribution of these pigments give hair its natural color.
In individuals with poliosis, there is a failure in the production or transfer of melanin to the keratinocytes, the cells that make up the hair shaft. This can result from a variety of factors including genetic mutations, autoimmune attacks on melanocytes, or trauma to the skin and hair follicles. While the underlying causes of poliosis are not fully understood, it is believed that dysfunctions in the melanocyte stem cells inside hair follicles play a significant role. Without these stem cells, there is no regeneration of melanocytes during the hair growth cycle, leading to the localized lack of pigmentation in hair fiber produced by the affected hair follicles.
Etiology of Poliosis: Poliosis can be congenital (present at birth) or acquired later in life. Both forms of poliosis may be associated with a wide range of conditions, and it is important to distinguish between benign and pathological causes. Poliosis can also be caused by some drug medications.
1. Congenital Poliosis: Congenital poliosis is often observed in association with genetic syndromes. Some of the most well-known syndromes include:
Waardenburg Syndrome : This is a group of genetic conditions that affect pigmentation and hearing. Waardenburg syndrome is caused by mutations in genes that regulate the development of melanocytes. Individuals with this syndrome may present with a white forelock, along with other pigmentation anomalies such as heterochromia (different-colored eyes) and patchy depigmentation of the skin. Sensorineural hearing loss is another hallmark of this condition.Tuberous Sclerosis : This genetic disorder is characterized by benign tumors in various organs, including the skin, brain, and kidneys. Some patients with tuberous sclerosis develop areas of depigmented hair, along with other skin manifestations such as hypomelanotic macules and angiofibromas.Piebaldism : A rare autosomal dominant condition, piebaldism is characterized by a lack of melanocytes in patches of skin and hair, resulting in localized depigmentation. The most common presentation is a white forelock, although other areas of the scalp or body may be affected. It is caused by mutations in the “KIT” gene, which is critical for melanocyte development.Other Genetic Conditions : Several other genetic conditions have been associated with poliosis, although findings have primarily been anecdotal and limited to case reports. These conditions include: Neurofibromatosis Type 1 (NF1) : This genetic disorder, which leads to the development of benign nerve tumors, has also been linked to poliosis in isolated case reports. NF1 is typically characterized by skin manifestations such as café-au-lait spots and freckling, but poliosis may appear in some patients as part of the pigmentary anomalies.Prolidase Deficiency : A rare metabolic disorder affecting collagen breakdown, prolidase deficiency can lead to various skin and systemic symptoms, including poliosis in some cases. The condition is typically associated with skin ulcers, recurrent infections, and intellectual disabilities.Tietze Syndrome : Though primarily a condition affecting the costal cartilages and presenting as chest pain, isolated reports have suggested that Tietze syndrome can also be associated with poliosis, although the mechanism remains unclear.Rubinstein-Taybi Syndrome : This genetic condition, associated with intellectual disability and distinctive facial features, has been linked to pigmentary anomalies, including poliosis, in a few case reports.Marfan Syndrome : An inherited disorder affecting connective tissue, Marfan syndrome is well known for its effects on skeletal, cardiovascular, and ocular systems. In rare instances, poliosis has also been reported as part of the clinical presentation. 2. Acquired Poliosis: Acquired poliosis may develop at any age and can be associated with various underlying conditions:
Vitiligo : This autoimmune disorder targets melanocytes, leading to depigmented patches of skin and hair. Poliosis can be a localized manifestation of vitiligo, affecting eyelashes, eyebrows, or scalp hair. The exact cause of the immune response in vitiligo remains unclear, but it is thought to involve both genetic predisposition and environmental triggers.Alopecia Areata : Alopecia areata is an autoimmune condition that leads to patchy hair loss. In some cases, when hair regrows, it may be white or gray due to a lack of melanocyte activity, resulting in poliosis. This is often a temporary phenomenon, and hair may regain its original color in subsequent cycles of growth.Inflammatory and Infectious Causes : Inflammatory skin conditions like psoriasis or dermatitis, as well as localized infections, can lead to damage to hair follicles and melanocytes. If melanocytes are selectively targeted or destroyed, the regrowth of hair in the affected area may lack pigment.Neurological Disorders : Certain neurological conditions, particularly those affecting the cranial nerves, have been associated with poliosis. For example, conditions like Vogt-Koyanagi-Harada syndrome (a rare multisystemic disorder) can lead to poliosis, along with other symptoms such as uveitis (inflammation of the eye), hearing loss, and skin depigmentation.Trauma and Burns : Physical trauma to the scalp or skin, including burns or surgical procedures, may disrupt melanocyte function, leading to poliosis in the affected area. In such cases, the hair may grow back without pigment due to localized melanocyte cell loss.Cancer and Neoplasms : Melanocytic destruction leading to poliosis can also occur in the setting of neoplasms, both benign and malignant. In adults, localized poliosis, especially on the scalp, should raise suspicion for melanoma, as melanocyte destruction in this context could indicate a malignancy. For instance, scalp melanoma can cause localized poliosis due to the immune response targeting melanocytes around the tumor.Halo Nevi: Halo nevi are benign melanocytic nevi that develop a depigmented halo surrounding them, likely due to an immune response against the nevus cells. When poliosis occurs over a halo nevus, it is believed to be part of this immune response, potentially affecting nearby hair follicles. The sudden appearance of poliosis in regions with halo nevi, particularly in children, may prompt clinical observation and sometimes histopathological examination.Neurofibromas: Poliosis has been reported in association with neurofibromas. Poliosis may rarely occur overlying solitary neurofibromas, which are benign tumors arising from nerve tissue. In a representative case, a child presented with localized swelling of the scalp that developed poliosis over time. Upon surgical excision, the swelling was identified as a neurofibroma. This example highlights how poliosis may indicate underlying neurofibromas or other neoplastic growths, signaling the need for further investigation. 3. Medication-Induced Poliosis : Several medications, both topical and systemic, have been associated with poliosis as a side effect, particularly in adults. These medications include:
Topical Medications : Prostaglandin Analogs (e.g., latanoprost) are commonly used for treating glaucoma and have been reported to cause poliosis, particularly in eyelashes, in a few case reports.Imiquimod , an immune response modifier often used in the treatment of actinic keratoses and superficial skin cancers, can sometimes result in depigmentation of hair in localized areas, according to a few case reports.Chloramphenicol , a topical antibiotic, has also been associated with poliosis in rare cases. Systemic Medications : Acitretin , a systemic retinoid used for psoriasis, and chloroquine , an antimalarial drug, have both been reported to cause poliosis occasionally.Cetuximab , a monoclonal antibody used in cancer therapy, and tumor-infiltrating lymphocyte (TIL) immunotherapy , also used in oncology, have been linked to changes in hair pigmentation, including poliosis in a few people. BRAF Inhibitors (BRAFI) and MEK Inhibitors (MEKI) : These medications are frequently used in both pediatric and adult oncology, particularly for refractory tumors. While not always causing true poliosis, BRAF and MEK inhibitors are known to induce changes in hair color, including progressive lightening. In one study, 29.5% of patients on BRAF inhibitors and 23.3% on MEK inhibitors experienced hair lightening, alopecia, or hair curling as side effects. The mechanisms by which these medications lead to poliosis or other hair pigment changes are not fully understood but are believed to involve the disruption of melanocyte activity either directly or through immune-mediated mechanisms. For instance, prostaglandin analogs may interfere with melanin production in the hair follicle, while immunotherapies such as TIL therapy may cause poliosis through immune responses that target melanocytes.
Diagnosis and Evaluation: When a patient presents with poliosis, a thorough clinical evaluation is essential to determine the underlying cause. The diagnosis is primarily clinical, based on the visual appearance of depigmented hair. However, additional investigations may be warranted depending on the suspected etiology.
Medical History and Physical Examination : A detailed history is critical in distinguishing between congenital and acquired poliosis. Physicians should inquire about any associated skin conditions, family history of genetic syndromes, autoimmune diseases, and recent infections or trauma.Dermatological Examination : A Wood’s lamp (ultraviolet light) examination may help identify associated depigmented skin areas, which may not be readily visible under normal lighting. In cases of suspected vitiligo, alopecia areata, or other inflammatory conditions, skin biopsies may be performed to assess the histopathology of the affected regions.Genetic Testing : For congenital causes such as Waardenburg syndrome or piebaldism, genetic testing may be necessary to confirm the diagnosis. Identifying specific mutations can help guide management and inform family planning.Autoimmune Screening : In cases of suspected autoimmune disorders like vitiligo or alopecia areata, autoimmune panels, including antinuclear antibody (ANA) tests, can sometimes be helpful to assess for other underlying conditions. This can aid in the management of poliosis if it is part of a broader autoimmune process. Management of Poliosis: Poliosis itself is a benign condition and does not typically require treatment unless it is causing psychological distress or is a cosmetic concern for the patient. However, addressing the underlying cause, if present, is important.
Cosmetic Solutions : For patients seeking treatment for aesthetic reasons, hair dyes can be used to mask the depigmented areas. It is essential to recommend products that are gentle and non-irritating to avoid further damage to the scalp and hair follicles.Treatment of Underlying Conditions : If poliosis is associated with an autoimmune condition like vitiligo or alopecia areata, treatment strategies should focus on controlling the underlying disease. Topical corticosteroids, immunosuppressants, or other targeted therapies may be beneficial in managing the broader condition, although they are unlikely to reverse poliosis.Psychological Support : For some individuals, poliosis can cause significant emotional distress, especially if it develops suddenly or in prominent areas like the scalp or face. Offering psychological support or counseling may be beneficial in helping patients cope with the cosmetic impact of the condition. Prognosis: The prognosis of poliosis depends on its underlying cause. In cases of congenital poliosis, the condition is permanent, as the melanocytes in affected areas are absent from birth. For acquired poliosis, the prognosis varies. In conditions like vitiligo or alopecia areata, poliosis may be temporary and resolve as the underlying disease is treated or enters remission. In other cases, such as trauma-induced poliosis, the condition may be permanent if melanocytes are irreversibly damaged.
Conclusion: Poliosis is a striking clinical feature that may be benign or indicative of a broader underlying condition. While the condition itself is harmless, understanding its etiology and addressing any associated disorders is critical for providing appropriate care. Genetic syndromes, autoimmune diseases, neurological conditions, and even trauma can all manifest as poliosis, and a thorough clinical evaluation is necessary to identify the underlying cause. Treatment is often focused on managing the primary condition, with cosmetic solutions available for those concerned about the aesthetic impact. As research continues, a deeper understanding of melanocyte biology and its dysregulation in conditions like poliosis may offer new avenues for treatment in the future.
Bibliography
11711645 {11711645:JIRRVQVC},{11711645:4NWTDDX8},{11711645:B7AWZXFA},{11711645:QTUZZ5DV},{11711645:XRQB9NQF},{11711645:JFS74TXF},{11711645:TR34GHFJ},{11711645:BJJ2SGSJ},{11711645:IJG9IA92},{11711645:N2JGXG3Z},{11711645:9CEEZUSB},{11711645:T6E5AHDX},{11711645:DB9J2AGI},{11711645:7IAXBTPX},{11711645:Q33ZHAE6},{11711645:KGDBHHDB},{11711645:FG6EG76C},{11711645:28JCNME4},{11711645:JGPJ5RI3},{11711645:BEGXBHS4},{11711645:RTDNXVE2},{11711645:MVBB6V8W},{11711645:27QFXMWC},{11711645:XX5BT68S},{11711645:3PN9RZEQ},{11711645:AZKJGFE8},{11711645:R3FJBMAK},{11711645:HGGNIA83} 1 vancouver 50 date asc 1635 https://www.keratin.com/wp-content/plugins/zotpress/ %7B%22status%22%3A%22success%22%2C%22updateneeded%22%3Afalse%2C%22instance%22%3Afalse%2C%22meta%22%3A%7B%22request_last%22%3A0%2C%22request_next%22%3A0%2C%22used_cache%22%3Atrue%7D%2C%22data%22%3A%5B%7B%22key%22%3A%22MVBB6V8W%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Fellman%20and%20Mehregan%22%2C%22parsedDate%22%3A%221976-04%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BFellman%20AC%2C%20Mehregan%20AH.%20Letter%3A%20Halo%20nevi%20of%20scalp%20with%20poliosis.%20Arch%20Dermatol.%201976%20Apr%3B112%284%29%3A559.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Letter%3A%20Halo%20nevi%20of%20scalp%20with%20poliosis%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22A.%20C.%22%2C%22lastName%22%3A%22Fellman%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22A.%20H.%22%2C%22lastName%22%3A%22Mehregan%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%221976-04%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%22%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%220003-987X%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A03%3A46Z%22%7D%7D%2C%7B%22key%22%3A%22JGPJ5RI3%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Herman%20et%20al.%22%2C%22parsedDate%22%3A%221991-07%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BHerman%20KL%2C%20Salman%20K%2C%20Rose%20LI.%20White%20forelock%20in%20Marfan%26%23x2019%3Bs%20syndrome%3A%20an%20unusual%20association%2C%20with%20review%20of%20the%20literature.%20Cutis.%201991%20July%3B48%281%29%3A82%26%23x2013%3B4.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22White%20forelock%20in%20Marfan%27s%20syndrome%3A%20an%20unusual%20association%2C%20with%20review%20of%20the%20literature%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22K.%20L.%22%2C%22lastName%22%3A%22Herman%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22K.%22%2C%22lastName%22%3A%22Salman%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22L.%20I.%22%2C%22lastName%22%3A%22Rose%22%7D%5D%2C%22abstractNote%22%3A%22The%20cutaneous%20expression%20of%20Marfan%26%23039%3Bs%20syndrome%20is%20generally%20limited%20to%20striae%20distensae%20and%20a%20number%20of%20uncommon%20associations%20with%20other%20dermatologic%20disorders.%20To%20date%2C%20there%20have%20been%20no%20reported%20cases%20of%20hair%20or%20nail%20abnormalities%20accompanying%20this%20disorder.%20We%20describe%20a%20patient%20with%20Marfan%26%23039%3Bs%20syndrome%20who%20presented%20with%20an%20acquired%20white%20forelock%20and%20we%20review%20the%20literature%20on%20the%20association%20of%20poliosis%20with%20various%20entities.%22%2C%22date%22%3A%221991-07%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%22%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%220011-4162%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A05%3A03Z%22%7D%7D%2C%7B%22key%22%3A%22BEGXBHS4%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Rathinam%20et%20al.%22%2C%22parsedDate%22%3A%221998-09%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BRathinam%20SR%2C%20Vijayalakshmi%20P%2C%20Namperumalsamy%20P%2C%20Nozik%20RA%2C%20Cunningham%20ET.%20Vogt-Koyanagi-Harada%20syndrome%20in%20children.%20Ocul%20Immunol%20Inflamm.%201998%20Sept%3B6%283%29%3A155%26%23x2013%3B61.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Vogt-Koyanagi-Harada%20syndrome%20in%20children%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22S.%20R.%22%2C%22lastName%22%3A%22Rathinam%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22P.%22%2C%22lastName%22%3A%22Vijayalakshmi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22P.%22%2C%22lastName%22%3A%22Namperumalsamy%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22R.%20A.%22%2C%22lastName%22%3A%22Nozik%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22E.%20T.%22%2C%22lastName%22%3A%22Cunningham%22%7D%5D%2C%22abstractNote%22%3A%22PURPOSE%3A%20To%20describe%20the%20clinical%20presentation%20and%20natural%20history%20of%20Vogt-Koyanagi-Harada%20%28VKH%29%20syndrome%20in%20children%2C%20an%20often%20unrecognized%20cause%20of%20pediatric%20uveitis.%5CnMETHODS%3A%20We%20performed%20a%20clinic-based%20cross-sectional%20survey%20and%20retrospective%20review%20of%20pediatric%20patients%20with%20VHK%20seen%20in%20the%20uveitis%20clinic%20at%20the%20Aravind%20Eye%20Hospital%2C%20Madurai%2C%20India%2C%20between%20January%201993%20and%20December%201995.%5CnRESULTS%3A%20A%20total%20of%2098%20patients%20with%20VKH%20syndrome%20were%20seen%20in%20the%20uveitis%20clinic%20at%20the%20Aravind%20Eye%20Hospital%20during%20the%20three%20years%20covered%20by%20the%20survey%2C%20of%20whom%20three%20%28about%203%25%2C%20with%20an%20approximate%20incidence%20of%201%20case%5C%2Fyear%29%20were%20children%2016%20years%20of%20age%20or%20younger.%20Initial%20symptoms%20included%20eye%20pain%2C%20redness%2C%20and%20blurred%20vision%20in%20all%20three%20patients.%20Headache%20and%20dysacusis%20accompanied%20the%20onset%20of%20visual%20symptoms%20in%20one%20patient.%20Each%20patient%20eventually%20developed%20areas%20of%20vitiligo%20and%20poliosis%2C%20although%20these%20signs%20were%20not%20present%20at%20the%20time%20of%20presentation%20in%20any%20of%20our%20patients.%20Signs%20of%20active%20uveitis%20included%20anterior%20chamber%20and%20vitreous%20inflammation%2C%20optic%20disc%20edema%2C%20exudative%20retinal%20detachments%2C%20and%20Dalen-Fuchs%26%23039%3B-like%20nodules.%20All%20three%20patients%20developed%20cataracts%2C%20two%20developed%20retinal%20pigment%20epithelium%20atrophy%2C%20and%20one%20developed%20glaucoma.%20Each%20patient%20responded%20well%2C%20with%20good%20visual%20recovery%2C%20to%20topical%20and%5C%2For%20systemic%20corticosteroids.%5CnCONCLUSIONS%3A%20Although%20frequently%20unrecognized%2C%20VKH%20syndrome%20may%20affect%20children.%20As%20with%20adults%2C%20visual%20loss%20occurs%20most%20typically%20as%20the%20result%20of%20cataract%2C%20glaucoma%2C%20or%20retinal%20pigment%20epithelium%20atrophy.%22%2C%22date%22%3A%221998-09%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1076%5C%2Focii.6.3.155.4041%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%220927-3948%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A04%3A31Z%22%7D%7D%2C%7B%22key%22%3A%2227QFXMWC%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Walker%20et%20al.%22%2C%22parsedDate%22%3A%221999-06%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BWalker%20S%2C%20Lucke%20TW%2C%20Burden%20AD%2C%20Thomson%20J.%20Poliosis%20circumscripta%20associated%20with%20scalp%20naevi%3A%20a%20report%20of%20four%20cases.%20Br%20J%20Dermatol.%201999%20June%3B140%286%29%3A1182%26%23x2013%3B4.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Poliosis%20circumscripta%20associated%20with%20scalp%20naevi%3A%20a%20report%20of%20four%20cases%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22S.%22%2C%22lastName%22%3A%22Walker%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22T.%20W.%22%2C%22lastName%22%3A%22Lucke%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22A.%20D.%22%2C%22lastName%22%3A%22Burden%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22J.%22%2C%22lastName%22%3A%22Thomson%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%221999-06%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%22%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%220007-0963%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A03%3A09Z%22%7D%7D%2C%7B%22key%22%3A%22BJJ2SGSJ%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Elston%20et%20al.%22%2C%22parsedDate%22%3A%222000-06%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BElston%20DM%2C%20Clayton%20AS%2C%20Meffert%20JJ%2C%20McCollough%20ML.%20Migratory%20poliosis%3A%20A%20forme%20fruste%20of%20alopecia%20areata%3F%20J%20Am%20Acad%20Dermatol.%202000%20June%3B42%286%29%3A1076%26%23x2013%3B7.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Migratory%20poliosis%3A%20A%20forme%20fruste%20of%20alopecia%20areata%3F%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22D.%20M.%22%2C%22lastName%22%3A%22Elston%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22A.%20S.%22%2C%22lastName%22%3A%22Clayton%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22J.%20J.%22%2C%22lastName%22%3A%22Meffert%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22M.%20L.%22%2C%22lastName%22%3A%22McCollough%22%7D%5D%2C%22abstractNote%22%3A%22We%20describe%20a%2019-year-old%20African-American%20man%20with%20a%2014-year%20history%20of%20migratory%20poliosis.%20We%20suggest%20that%20this%20phenomenon%20may%20represent%20a%20forme%20fruste%20of%20alopecia%20areata.%22%2C%22date%22%3A%222000-06%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1016%5C%2Fs0190-9622%2800%2990307-4%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%220190-9622%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A13%3A27Z%22%7D%7D%2C%7B%22key%22%3A%22IJG9IA92%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Wu%20et%20al.%22%2C%22parsedDate%22%3A%222006-02%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BWu%20JJ%2C%20Huang%20DB%2C%20Tyring%20SK.%20Postherpetic%20poliosis.%20Arch%20Dermatol.%202006%20Feb%3B142%282%29%3A250%26%23x2013%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Postherpetic%20poliosis%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jashin%20J.%22%2C%22lastName%22%3A%22Wu%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22David%20B.%22%2C%22lastName%22%3A%22Huang%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Stephen%20K.%22%2C%22lastName%22%3A%22Tyring%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222006-02%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1001%5C%2Farchderm.142.2.250%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%220003-987X%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A12%3A59Z%22%7D%7D%2C%7B%22key%22%3A%22RTDNXVE2%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Young%20et%20al.%22%2C%22parsedDate%22%3A%222008-02-28%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BYoung%20LC%2C%20Van%20Dyke%20GS%2C%20Lipton%20S%2C%20Binder%20SW.%20Poliosis%20overlying%20a%20nevus%20with%20blue%20nevus%20features.%20Dermatol%20Online%20J.%202008%20Feb%2028%3B14%282%29%3A20.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Poliosis%20overlying%20a%20nevus%20with%20blue%20nevus%20features%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Lorraine%20C.%22%2C%22lastName%22%3A%22Young%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Gregory%20S.%22%2C%22lastName%22%3A%22Van%20Dyke%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Shira%22%2C%22lastName%22%3A%22Lipton%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Scott%20W.%22%2C%22lastName%22%3A%22Binder%22%7D%5D%2C%22abstractNote%22%3A%22Poliosis%20is%20a%20localized%20patch%20of%20gray%20or%20white%20hair.%20Because%20it%20can%20be%20seen%20with%20a%20variety%20of%20disorders%20and%20drugs%2C%20a%20full%20history%20and%20exam%20is%20indicated.%20Additionally%2C%20it%20can%20be%20associated%20with%20underlying%20benign%20and%20malignant%20tumors%2C%20necessitating%20histological%20identification.%20We%20review%20the%20lesions%20that%20are%20reported%20with%20poliosis.%20In%20addition%2C%20we%20will%20report%20a%20case%20of%20poliosis%20overlying%20an%20intradermal%20nevus%20with%20congenital%20as%20well%20as%20blue%20nevus%20features.%20To%20the%20best%20of%20our%20knowledge%2C%20blue%20nevus%20features%20associated%20with%20poliosis%20have%20not%20been%20previously%20described.%22%2C%22date%22%3A%222008-02-28%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%22%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221087-2108%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A04%3A10Z%22%7D%7D%2C%7B%22key%22%3A%22T6E5AHDX%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Jacob%20and%20Blyumin%22%2C%22parsedDate%22%3A%222008-06%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BJacob%20SE%2C%20Blyumin%20M.%20Vitiligo-like%20hypopigmentation%20with%20poliosis%20following%20treatment%20of%20superficial%20basal%20cell%20carcinoma%20with%20imiquimod.%20Dermatol%20Surg.%202008%20June%3B34%286%29%3A844%26%23x2013%3B5.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Vitiligo-like%20hypopigmentation%20with%20poliosis%20following%20treatment%20of%20superficial%20basal%20cell%20carcinoma%20with%20imiquimod%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Sharon%20E.%22%2C%22lastName%22%3A%22Jacob%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mariana%22%2C%22lastName%22%3A%22Blyumin%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222008-06%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1111%5C%2Fj.1524-4725.2008.34158.x%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221524-4725%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A12%3A20Z%22%7D%7D%2C%7B%22key%22%3A%22DB9J2AGI%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Tan%20and%20Zhu%22%2C%22parsedDate%22%3A%222010%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BTan%20C%2C%20Zhu%20WY.%20Permanent%20poliosis%20following%20repetitive%20plucking%20in%20an%20adolescent.%20J%20Cutan%20Med%20Surg.%202010%3B14%284%29%3A193%26%23x2013%3B4.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Permanent%20poliosis%20following%20repetitive%20plucking%20in%20an%20adolescent%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Cheng%22%2C%22lastName%22%3A%22Tan%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Wen-Yuan%22%2C%22lastName%22%3A%22Zhu%22%7D%5D%2C%22abstractNote%22%3A%22BACKGROUND%20AND%20OBJECTIVE%3A%20poliosis%20is%20an%20inherited%20or%20acquired%20loss%20of%20pigment%20from%20a%20group%20of%20closely%20positioned%20hair%20follicles%20characterized%20by%20a%20patch%20of%20white%20hair.%20It%20is%20commonly%20seen%20in%20vitiligo%2C%20piebaldism%2C%20Waardenburg%20syndrome%2C%20Vogt-Koyanagi-Harada%20syndrome%2C%20Griscelli%20syndrome%2C%20and%20Apert%20syndrome.%20We%20investigated%20a%20male%20manifesting%20poliosis%20on%20the%20chin%20after%20repetitive%20plucking.%5CnCONCLUSION%3A%20to%20our%20knowledge%2C%20poliosis%20induced%20by%20repeated%20plucking%20has%20never%20been%20documented.%22%2C%22date%22%3A%222010%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.2310%5C%2F7750.2010.09062%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221203-4754%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A12%3A04Z%22%7D%7D%2C%7B%22key%22%3A%22XX5BT68S%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Bernardes%20and%20Bonfioli%22%2C%22parsedDate%22%3A%222010-05%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BBernardes%20TF%2C%20Bonfioli%20AA.%20Blepharitis.%20Semin%20Ophthalmol.%202010%20May%3B25%283%29%3A79%26%23x2013%3B83.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Blepharitis%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Taliana%20Freitas%22%2C%22lastName%22%3A%22Bernardes%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Adriana%20Alvim%22%2C%22lastName%22%3A%22Bonfioli%22%7D%5D%2C%22abstractNote%22%3A%22Blepharitis%20is%20a%20chronic%20inflammatory%20process%20of%20the%20eyelid%20margin.%20It%20is%20a%20common%20eye%20disorder%20throughout%20the%20world%20and%20can%20affect%20any%20age%20group.%20It%20may%20be%20associated%20with%20several%20systemic%20diseases%2C%20particularly%20rosacea%20and%20seborrheic%20dermatitis%2C%20and%20is%20related%20to%20other%20ocular%20conditions%20like%20dry%20eye%2C%20chalazion%2C%20conjunctivitis%2C%20and%20keratitis.%20Common%20symptoms%20associated%20with%20blepharitis%20are%20burning%20sensation%2C%20irritation%2C%20tearing%2C%20photophobia%2C%20blurred%20vision%2C%20and%20red%20eyes.%20Clinical%20examination%20reveals%20the%20presence%20of%20scurf%2C%20telangiectatic%20vascular%20changes%20of%20the%20eyelid%20margin%2C%20inspissated%20meibomian%20glands%2C%20conjuntival%20hyperemia%2C%20punctuate%20keratopathy%2C%20cornea%20vascularization%2C%20and%20ulceration.%20Patients%20with%20longstanding%20chronic%20blepharitis%20may%20present%20hypertrophy%20of%20the%20lid%20margin%2C%20scars%2C%20madarosis%2C%20trichiasis%2C%20and%20poliosis.%20Treatment%20of%20blepharitis%20is%20long%20and%20unsatisfactory.%20Long-term%20commitment%20to%20eyelid%20hygiene%20is%20essential.%20Other%20treatment%20options%20are%20discussed.%22%2C%22date%22%3A%222010-05%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.3109%5C%2F08820538.2010.488562%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221744-5205%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A02%3A57Z%22%7D%7D%2C%7B%22key%22%3A%227IAXBTPX%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Chappell%20et%20al.%22%2C%22parsedDate%22%3A%222012-02%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BChappell%20JA%2C%20Chu%20MB%2C%20Martin%20K%2C%20Hurley%20MY.%20Acitretin-induced%20poliosis%20with%20concurrent%20alopecia.%20J%20Drugs%20Dermatol.%202012%20Feb%3B11%282%29%3A247%26%23x2013%3B9.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Acitretin-induced%20poliosis%20with%20concurrent%20alopecia%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jeaneen%20A.%22%2C%22lastName%22%3A%22Chappell%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Melinda%20B.%22%2C%22lastName%22%3A%22Chu%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Katherine%22%2C%22lastName%22%3A%22Martin%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22M.%20Yadira%22%2C%22lastName%22%3A%22Hurley%22%7D%5D%2C%22abstractNote%22%3A%22Acitretin%2C%20a%20metabolite%20of%20the%20aromatic%20retinoid%20etretinate%2C%20has%20been%20utilized%20successfully%20in%20the%20treatment%20of%20psoriasis%20since%20the%20late%201980s.%20Of%20the%20oral%20retinoids%20available%2C%20etretinate%20and%20acitretin%20are%20the%20most%20likely%20agents%20to%20induce%20various%20dose-dependent%20hair%20changes%2C%20but%20to%20our%20knowledge%20this%20is%20the%20first%20reported%20case%20of%20acitretin-induced%20poliosis.%20Additional%20cutaneous%20findings%20included%20skin%20atrophy%20and%20stickiness.%20Here%20we%20report%20a%20case%20of%20full%20body%20acitretin-induced%20poliosis%20with%20concurrent%20alopecia%20in%20a%20patient%20with%20psoriasis.%20A%20proposed%20mechanism%20for%20the%20poliosis%20is%20also%20presented%20here.%20Closer%20examination%20of%20retinoid-induced%20hair%20changes%20is%20needed%20in%20order%20to%20help%20physicians%20better%20counsel%20their%20patients%20regarding%20the%20adverse%20effects%20of%20acitretin%20and%20to%20expand%20the%20current%20knowledge%20on%20hair%20follicle%20biology.%22%2C%22date%22%3A%222012-02%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%22%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221545-9616%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A11%3A52Z%22%7D%7D%2C%7B%22key%22%3A%22Q33ZHAE6%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Awad%22%2C%22parsedDate%22%3A%222013-03%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BAwad%20SS.%20Repigmentation%20of%20poliosis%20after%20epithelial%20grafting%20for%20vitiligo.%20Dermatol%20Surg.%202013%20Mar%3B39%283%20Pt%201%29%3A406%26%23x2013%3B11.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Repigmentation%20of%20poliosis%20after%20epithelial%20grafting%20for%20vitiligo%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Sherif%20S.%22%2C%22lastName%22%3A%22Awad%22%7D%5D%2C%22abstractNote%22%3A%22BACKGROUND%3A%20Vitiligo%20is%20a%20disease%20of%20color%20loss%20from%20skin%20and%20possibly%20also%20from%20hair.%20The%20presence%20of%20white%20hair%20follicles%20is%20known%20to%20be%20a%20bad%20prognostic%20sign.%5CnOBJECTIVES%3A%20To%20evaluate%20the%20possibility%20of%20repigmentation%20of%20white%20hair%20follicles%20after%20epithelial%20grafting.%5CnMETHODS%3A%20Patients%20with%20recalcitrant%20vitiligo%20with%20loss%20of%20hair%20pigment%20were%20treated%20using%20Chinese%20cupping%20blisters%20or%20ultrathin%20Thiersch%20grafting%20after%20de-epithelialization%20of%20vitiliginous%20patches%20by%20dermabrasion.%20Phototherapy%20was%20used%20afterward%20to%20enhance%20success.%5CnRESULTS%3A%20Repigmentation%20of%20the%20skin%20surface%20was%20obtained%20with%20as%20little%20as%201%20to%202%5Cu00a0months%20of%20phototherapy%2C%20as%20expected%2C%20and%20further%20follow-up%20of%20cases%20revealed%20the%20re-coloring%20of%20hair%20follicles%20after%204%20to%2011%5Cu00a0months.%5CnCONCLUSION%3A%20Re-coloring%20of%20poliosis%20with%20vitiligo%20is%20possible%20but%20was%20unexpected%20because%20of%20the%20difference%20in%20mechanism%20and%20signaling%20required%20between%20hair%20bulb%20melanization%20and%20the%20surface%20skin.%20One%20likely%20mechanism%20to%20explain%20this%20change%20is%20that%20melanocyte%20stem%20cells%20are%20stimulated%20and%20migrate%20to%20supply%20hair%20bulbs%20with%20new%20mature%20melanocytes.%20Epithelial%20grafting%20of%20vitiligo%20with%20poliosis%20in%20hairy%20areas%20should%20be%20a%20treatment%20of%20choice%20when%20white%20hair%20tufts%20cause%20cosmetic%20disfigurement.%22%2C%22date%22%3A%222013-03%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1111%5C%2Fdsu.12082%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221524-4725%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A11%3A39Z%22%7D%7D%2C%7B%22key%22%3A%223PN9RZEQ%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Sleiman%20et%20al.%22%2C%22parsedDate%22%3A%222013-10%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BSleiman%20R%2C%20Kurban%20M%2C%20Succaria%20F%2C%20Abbas%20O.%20Poliosis%20circumscripta%3A%20overview%20and%20underlying%20causes.%20J%20Am%20Acad%20Dermatol.%202013%20Oct%3B69%284%29%3A625%26%23x2013%3B33.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Poliosis%20circumscripta%3A%20overview%20and%20underlying%20causes%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Rima%22%2C%22lastName%22%3A%22Sleiman%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mazen%22%2C%22lastName%22%3A%22Kurban%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Farah%22%2C%22lastName%22%3A%22Succaria%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ossama%22%2C%22lastName%22%3A%22Abbas%22%7D%5D%2C%22abstractNote%22%3A%22Although%20traditionally%20known%20as%20%26quot%3Bwhite%20forelock%2C%26quot%3B%20poliosis%20circumscripta%2C%20defined%20as%20a%20localized%20patch%20of%20white%20hair%20in%20a%20group%20of%20hair%20follicles%2C%20can%20involve%20any%20hairy%20area%20on%20the%20body%20including%20the%20scalp%2C%20eyebrows%2C%20and%20eyelashes.%20Microscopically%2C%20poliosis%20demonstrates%20either%20decreased%20or%20absent%20melanin%20and%5C%2For%20melanocytes%20in%20the%20hair%20bulbs%20of%20the%20affected%20hair%20follicles.%20Classically%2C%20poliosis%20is%20known%20to%20occur%20in%20the%20setting%20of%20several%20genetic%20syndromes%20including%20piebaldism%2C%20Waardenburg%2C%20and%20tuberous%20sclerosis.%20In%20addition%2C%20poliosis%20has%20been%20described%20in%20association%20with%20various%20acquired%20conditions.%20These%20include%20inflammatory%20conditions%2C%20benign%20and%20malignant%20neoplastic%20entities%20that%20are%20mainly%20melanocytic%2C%20medications%2C%20and%20others.%20In%20this%20review%2C%20we%20aim%20to%20describe%20the%20different%20conditions%20where%20poliosis%20may%20be%20encountered%2C%20with%20the%20aim%20of%20helping%20the%20clinician%20to%20better%20evaluate%20any%20patient%20presenting%20with%20poliosis.%22%2C%22date%22%3A%222013-10%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.jaad.2013.05.022%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221097-6787%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A02%3A27Z%22%7D%7D%2C%7B%22key%22%3A%229CEEZUSB%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Malik%20et%20al.%22%2C%22parsedDate%22%3A%222014-02%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BMalik%20TG%2C%20Khalil%20M%2C%20Bhatti%20MM.%20Pityriasis%20alba%20with%20poliosis.%20J%20Coll%20Physicians%20Surg%20Pak.%202014%20Feb%3B24%282%29%3A138%26%23x2013%3B40.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Pityriasis%20alba%20with%20poliosis%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Tayyaba%20Gul%22%2C%22lastName%22%3A%22Malik%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Muhammad%22%2C%22lastName%22%3A%22Khalil%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Muhammad%20Moeen%22%2C%22lastName%22%3A%22Bhatti%22%7D%5D%2C%22abstractNote%22%3A%22Pityriasis%20alba%20is%20a%20skin%20disease%2C%20commonly%20seen%20in%20children%20and%20young%20adults.%20This%20case%20presents%20the%20ocular%20association%20of%20this%20disease%20in%20a%2010%20years%20old%20Pakistani%20male.%20Ocular%20features%20in%20this%20case%20were%20poliosis%2C%20tilted%20disc%2C%20high%20myopia%20and%20chorioretinal%20degeneration.%20Tilted%20discs%20and%20high%20myopia%20can%20be%20coincidental%20but%20poliosis%20and%20decreased%20pigment%20in%20retinal%20pigment%20epithelium%20are%20closely%20related%20with%20the%20hypopigmentation%20seen%20in%20this%20disease.%22%2C%22date%22%3A%222014-02%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%22%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221681-7168%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A12%3A33Z%22%7D%7D%2C%7B%22key%22%3A%22KGDBHHDB%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Feng%20et%20al.%22%2C%22parsedDate%22%3A%222014-07%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BFeng%20H%2C%20Sun%20Y%2C%20Wang%20Q.%20Downregulation%20of%20c-Kit%5C%2FMITF-M%20in%20graying%20hair%20of%20juvenile%20poliosis.%20Acta%20Derm%20Venereol.%202014%20July%3B94%284%29%3A484%26%23x2013%3B5.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Downregulation%20of%20c-Kit%5C%2FMITF-M%20in%20graying%20hair%20of%20juvenile%20poliosis%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Hua%22%2C%22lastName%22%3A%22Feng%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Yina%22%2C%22lastName%22%3A%22Sun%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Qi%22%2C%22lastName%22%3A%22Wang%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222014-07%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.2340%5C%2F00015555-1763%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221651-2057%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A11%3A24Z%22%7D%7D%2C%7B%22key%22%3A%22HGGNIA83%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Jalalat%20et%20al.%22%2C%22parsedDate%22%3A%222014-09-16%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BJalalat%20SZ%2C%20Kelsoe%20JR%2C%20Cohen%20PR.%20Alopecia%20areata%20with%20white%20hair%20regrowth%3A%20case%20report%20and%20review%20of%20poliosis.%20Dermatol%20Online%20J.%202014%20Sept%2016%3B20%289%29%3A13030%5C%2Fqt1xk5b26v.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Alopecia%20areata%20with%20white%20hair%20regrowth%3A%20case%20report%20and%20review%20of%20poliosis%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Sheila%20Z.%22%2C%22lastName%22%3A%22Jalalat%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22John%20R.%22%2C%22lastName%22%3A%22Kelsoe%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Philip%20R.%22%2C%22lastName%22%3A%22Cohen%22%7D%5D%2C%22abstractNote%22%3A%22Alopecia%20areata%20is%20thought%20to%20be%20a%20T-cell%20mediated%20and%20cytokine%20mediated%20autoimmune%20disease%20that%20results%20in%20non-scarring%20hair%20loss.%20Poliosis%20has%20been%20described%20as%20a%20localized%20depigmentation%20of%20hair%20caused%20by%20a%20deficiency%20of%20melanin%20in%20hair%20follicles.%20A%2057-year-old%20man%20with%20a%20history%20of%20alopecia%20areata%20developed%20white%20hair%20regrowth%20in%20areas%20of%20previous%20hair%20loss.%20We%20retrospectively%20reviewed%20the%20medical%20literature%20using%20PubMed%2C%20searching%3A%20%281%29%20alopecia%20areata%20and%20%282%29%20poliosis.%20Poliosis%20may%20be%20associated%20with%20autoimmune%20diseases%20including%20alopecia%20areata%2C%20as%20described%20in%20our%20case.%20However%2C%20it%20is%20also%20reported%20in%20patients%20who%20have%20cutaneous%20lesions%2C%20genetic%20syndromes%2C%20infections%2C%20medication%20use%2C%20and%20trauma.%20Hair%20regrowth%20following%20alopecia%20areata%20may%20be%20associated%20with%20poliosis.%20We%20hypothesize%20that%20the%20incidence%20of%20poliosis%20in%20areas%20of%20previous%20alopecia%20areata-related%20hair%20loss%20may%20be%20greater%20than%20reflected%20in%20the%20published%20literature.%22%2C%22date%22%3A%222014-09-16%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%22%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221087-2108%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A01%3A30Z%22%7D%7D%2C%7B%22key%22%3A%22N2JGXG3Z%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22%5Cu00d6zyurt%20and%20%5Cu00c7etinkaya%22%2C%22parsedDate%22%3A%222015%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3B%26%23xD6%3Bzyurt%20S%2C%20%26%23xC7%3Betinkaya%20GS.%20Hypertrichosis%20of%20the%20malar%20areas%20and%20poliosis%20of%20the%20eyelashes%20caused%20by%20latanoprost.%20Actas%20Dermosifiliogr.%202015%3B106%281%29%3A74%26%23x2013%3B5.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Hypertrichosis%20of%20the%20malar%20areas%20and%20poliosis%20of%20the%20eyelashes%20caused%20by%20latanoprost%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22S.%22%2C%22lastName%22%3A%22%5Cu00d6zyurt%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22G.%20Seyman%22%2C%22lastName%22%3A%22%5Cu00c7etinkaya%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222015%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.ad.2014.05.005%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221578-2190%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A12%3A47Z%22%7D%7D%2C%7B%22key%22%3A%22AZKJGFE8%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Grob%20and%20Grekin%22%2C%22parsedDate%22%3A%222016-02%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BGrob%20A%2C%20Grekin%20S.%20Piebaldism%20in%20children.%20Cutis.%202016%20Feb%3B97%282%29%3A90%26%23x2013%3B2.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Piebaldism%20in%20children%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Alexandra%22%2C%22lastName%22%3A%22Grob%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Steven%22%2C%22lastName%22%3A%22Grekin%22%7D%5D%2C%22abstractNote%22%3A%22Piebaldism%20is%20a%20rare%20autosomal-dominant%20disorder%20of%20melanocyte%20development%20characterized%20by%20congenital%20poliosis%20and%20stable%20patches%20of%20leukoderma.%20Initially%2C%20these%20clinical%20features%20may%20be%20the%20presenting%20signs%20of%20various%20syndromes%20or%20associated%20diseases%2C%20which%20should%20be%20considered%20in%20the%20differential%20diagnosis.%20We%20present%20the%20case%20of%20a%2014-year-old%20adolescent%20girl%20with%20piebaldism%2C%20along%20with%20a%20review%20of%20the%20pathogenesis%2C%20diagnosis%2C%20and%20management%20of%20this%20disease%20entity.%22%2C%22date%22%3A%222016-02%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%22%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%222326-6929%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A01%3A58Z%22%7D%7D%2C%7B%22key%22%3A%22TR34GHFJ%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Lee%20et%20al.%22%2C%22parsedDate%22%3A%222019-06%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BLee%20YB%2C%20Jun%20M%2C%20Lee%20WS.%20Alopecia%20areata%20and%20poliosis%3A%20A%20retrospective%20analysis%20of%20258%20cases.%20J%20Am%20Acad%20Dermatol.%202019%20June%3B80%286%29%3A1776%26%23x2013%3B8.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Alopecia%20areata%20and%20poliosis%3A%20A%20retrospective%20analysis%20of%20258%20cases%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Young%20Bin%22%2C%22lastName%22%3A%22Lee%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Myungsoo%22%2C%22lastName%22%3A%22Jun%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Won-Soo%22%2C%22lastName%22%3A%22Lee%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222019-06%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.jaad.2018.11.033%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221097-6787%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A13%3A41Z%22%7D%7D%2C%7B%22key%22%3A%22JFS74TXF%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Schollenberger%20et%20al.%22%2C%22parsedDate%22%3A%222019-12%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BSchollenberger%20MD%2C%20Stein%20JE%2C%20Taube%20JM%2C%20Lipson%20EJ.%20Poliosis%20Circumscripta%3A%20A%20Mark%20of%20Melanoma.%20Am%20J%20Med.%202019%20Dec%3B132%2812%29%3A1417%26%23x2013%3B8.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Poliosis%20Circumscripta%3A%20A%20Mark%20of%20Melanoma%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Megan%20D.%22%2C%22lastName%22%3A%22Schollenberger%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Julie%20E.%22%2C%22lastName%22%3A%22Stein%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Janis%20M.%22%2C%22lastName%22%3A%22Taube%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Evan%20J.%22%2C%22lastName%22%3A%22Lipson%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222019-12%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.amjmed.2019.05.042%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221555-7162%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A13%3A57Z%22%7D%7D%2C%7B%22key%22%3A%22B7AWZXFA%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Burzi%20et%20al.%22%2C%22parsedDate%22%3A%222021-07%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BBurzi%20L%2C%20Parietti%20M%2C%20Agostini%20A%2C%20Marra%20E%2C%20Fierro%20MT%2C%20Ribero%20S%2C%20et%20al.%20Eyelashes%20poliosis%20as%20first%20sign%20of%20metastatic%20melanoma.%20J%20Eur%20Acad%20Dermatol%20Venereol.%202021%20July%3B35%287%29%3Ae459%26%23x2013%3B60.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Eyelashes%20poliosis%20as%20first%20sign%20of%20metastatic%20melanoma%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22L.%22%2C%22lastName%22%3A%22Burzi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22M.%22%2C%22lastName%22%3A%22Parietti%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22A.%22%2C%22lastName%22%3A%22Agostini%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22E.%22%2C%22lastName%22%3A%22Marra%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22M.%20T.%22%2C%22lastName%22%3A%22Fierro%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22S.%22%2C%22lastName%22%3A%22Ribero%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22P.%22%2C%22lastName%22%3A%22Quaglino%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222021-07%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1111%5C%2Fjdv.17215%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221468-3083%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A14%3A58Z%22%7D%7D%2C%7B%22key%22%3A%22R3FJBMAK%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Hong%20et%20al.%22%2C%22parsedDate%22%3A%222022-10-24%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BHong%20JY%2C%20Ahn%20HK%2C%20Kim%20S%2C%20Lee%20SH.%20Paediatric%20Poliosis%20as%20the%20Presenting%20Feature%20of%20Scalp%20Vitiligo%3A%20A%20Retrospective%20Case%20Series.%20Acta%20Derm%20Venereol.%202022%20Oct%2024%3B102%3Aadv00800.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Paediatric%20Poliosis%20as%20the%20Presenting%20Feature%20of%20Scalp%20Vitiligo%3A%20A%20Retrospective%20Case%20Series%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ji%20Yeon%22%2C%22lastName%22%3A%22Hong%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Hyun%20Keun%22%2C%22lastName%22%3A%22Ahn%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Sungbum%22%2C%22lastName%22%3A%22Kim%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Si-Hyung%22%2C%22lastName%22%3A%22Lee%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222022-10-24%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.2340%5C%2Factadv.v102.2492%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221651-2057%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A01%3A45Z%22%7D%7D%2C%7B%22key%22%3A%224NWTDDX8%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Rodrigues%20and%20Mendonca%22%2C%22parsedDate%22%3A%222023-04%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BRodrigues%20G%2C%20Mendonca%20T.%20Eyelash%20poliosis%20associated%20with%20Vogt-Koyanagi%20Harada%20disease.%20Clin%20Exp%20Optom.%202023%20Apr%3B106%283%29%3A338%26%23x2013%3B9.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Eyelash%20poliosis%20associated%20with%20Vogt-Koyanagi%20Harada%20disease%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Gladys%22%2C%22lastName%22%3A%22Rodrigues%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Teena%22%2C%22lastName%22%3A%22Mendonca%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222023-04%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1080%5C%2F08164622.2022.2029681%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221444-0938%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A15%3A10Z%22%7D%7D%2C%7B%22key%22%3A%22QTUZZ5DV%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Nemovi%20et%20al.%22%2C%22parsedDate%22%3A%222023-07%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BNemovi%20K%2C%20Jamali%20A%2C%20Matinpour%20K%2C%20Dasanu%20CA.%20Widespread%20vitiligo%20and%20poliosis%20following%20ipilimumab-nivolumab%20combination%20therapy.%20J%20Oncol%20Pharm%20Pract.%202023%20July%3B29%285%29%3A1278%26%23x2013%3B82.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Widespread%20vitiligo%20and%20poliosis%20following%20ipilimumab-nivolumab%20combination%20therapy%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Khashayar%22%2C%22lastName%22%3A%22Nemovi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Arsia%22%2C%22lastName%22%3A%22Jamali%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Keyan%22%2C%22lastName%22%3A%22Matinpour%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Constantin%20A.%22%2C%22lastName%22%3A%22Dasanu%22%7D%5D%2C%22abstractNote%22%3A%22INTRODUCTION%3A%20Combined%20immune%20checkpoint%20inhibitor%20therapy%20has%20been%20successfully%20used%20in%20the%20treatment%20of%20several%20malignancies.%20Adverse%20effects%20with%20the%20combination%20therapy%20may%20be%20more%20severe%20than%20the%20ones%20seen%20with%20single%20immune%20checkpoint%20inhibitors.%5CnCASE%20PRESENTATION%3A%20We%20report%20a%20unique%20case%20of%20a%2059-year-old%20man%20of%20dark%20skin%20complexion%20who%20underwent%20treatment%20with%20intravenous%20ipilimumab-nivolumab%20every%203%20weeks%20for%20metastatic%20malignant%20melanoma.%20After%20three%20cycles%20of%20this%20therapy%2C%20he%20developed%20extensive%20skin%20depigmentation%20that%20within%206%20weeks%2C%20affected%20nearly%20the%20entire%20skin%20surface%2C%20along%20with%20progressive%20poliosis.%5CnMANAGEMENT%20AND%20OUTCOME%3A%20Ipilimumab-nivolumab%20therapy%20was%20subsequently%20discontinued%20due%20to%20grade%203%20enterocolitis%20requiring%20high-dose%20steroids%20and%20intravenous%20infliximab.%20About%20six%20months%20later%2C%20imaging%20studies%20showed%20a%20relapse%20of%20malignant%20melanoma.%20At%20that%20juncture%2C%20vitiligo%20affected%20the%20total%20body%20surface%20area%2C%20resembling%20albinism%2C%20along%20with%20near-total%20poliosis%20and%20significant%20photosensitivity.%20Pembrolizumab%20was%20tried%20but%20had%20to%20be%20stopped%20after%20three%20cycles%20due%20to%20the%20reoccurrence%20of%20grade%203%20enterocolitis.%20Progression%20of%20malignant%20melanoma%20with%20new%20brain%2C%20lung%2C%20liver%2C%20subcutaneous%2C%20and%20colonic%20metastases%20led%20to%20the%20patient%26%23039%3Bs%20demise.%5CnCONCLUSION%3A%20We%20report%20a%20unique%20case%20of%20severe%20vitiligo%20and%20poliosis%20that%20involved%20total%20body%20surface%20area%20in%20a%20Caucasian%20man%20with%20dark%20complexion%2C%20resembling%20albinism.%20Further%20studies%20are%20warranted%20to%20evaluate%20the%20severity%20of%20dermatologic%20side%20effects%20with%20combination%20immune%20checkpoint%20inhibitor%20therapy.%22%2C%22date%22%3A%222023-07%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1177%5C%2F10781552231154460%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221477-092X%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A14%3A43Z%22%7D%7D%2C%7B%22key%22%3A%22XRQB9NQF%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Karch%20et%20al.%22%2C%22parsedDate%22%3A%222023-12-01%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BKarch%20JL%2C%20Davis%20MJ%2C%20Momtahen%20S%2C%20Simmons%20BJ.%20Subcutaneous%20Nodule%20With%20Poliosis%3A%20An%20Unusual%20Presentation%20of%20Melanoma%20Ex%20Blue%20Nevus.%20Dermatol%20Surg.%202023%20Dec%201%3B49%2812%29%3A1206%26%23x2013%3B7.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Subcutaneous%20Nodule%20With%20Poliosis%3A%20An%20Unusual%20Presentation%20of%20Melanoma%20Ex%20Blue%20Nevus%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jamie%20L.%22%2C%22lastName%22%3A%22Karch%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Matthew%20J.%22%2C%22lastName%22%3A%22Davis%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Shabnam%22%2C%22lastName%22%3A%22Momtahen%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Brian%20J.%22%2C%22lastName%22%3A%22Simmons%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222023-12-01%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1097%5C%2FDSS.0000000000003951%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221524-4725%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A14%3A12Z%22%7D%7D%2C%7B%22key%22%3A%2228JCNME4%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Rangu%20and%20Oza%22%2C%22parsedDate%22%3A%222024%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BRangu%20SA%2C%20Oza%20VS.%20Poliosis%2C%20hair%20pigment%20dilution%2C%20and%20premature%20graying%20of%20the%20hair%3A%20A%20diagnostic%20approach%20in%20pediatric%20patients%20and%20review%20of%20the%20literature.%20Pediatr%20Dermatol.%202024%3B41%282%29%3A197%26%23x2013%3B203.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Poliosis%2C%20hair%20pigment%20dilution%2C%20and%20premature%20graying%20of%20the%20hair%3A%20A%20diagnostic%20approach%20in%20pediatric%20patients%20and%20review%20of%20the%20literature%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Sneha%20A.%22%2C%22lastName%22%3A%22Rangu%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Vikash%20S.%22%2C%22lastName%22%3A%22Oza%22%7D%5D%2C%22abstractNote%22%3A%22Poliosis%20is%20defined%20as%20the%20absence%20of%20melanin%20in%20hair%2C%20and%20hair%20graying%20typically%20occurs%20with%20hair%20melanin%20reduction.%20Poliosis%20can%20occur%20at%20any%20age%20but%20presents%20in%20childhood%20in%20certain%20genetic%20and%20acquired%20conditions%2C%20with%20many%20families%20seeking%20evaluation%20from%20a%20pediatric%20dermatologist.%20Poliosis%20presents%20as%20white%20hair%20typically%20restricted%20to%20a%20certain%20location%20of%20the%20scalp.%20Children%20may%20also%20present%20with%20a%20reduction%20of%20expected%20hair%20pigmentation%2C%20referred%20to%20as%20pigment%20dilution%2C%20or%20the%20development%20of%20hair%20graying.%20This%20review%20aims%20to%20provide%20a%20streamlined%20diagnostic%20approach%20for%20pediatric%20dermatologists%20when%20presented%20with%20these%20hair%20findings.%20Poliosis%20should%20be%20recognized%20as%20a%20potential%20diagnostic%20feature%20or%20initial%20sign%20in%20many%20syndromes%20and%20thus%20can%20guide%20clinicians%20in%20diagnosing%20and%20managing%20conditions%20earlier%20in%20a%20patient%26%23039%3Bs%20care.%20Since%20many%20of%20the%20genetic%20and%20acquired%20conditions%20that%20present%20with%20poliosis%20or%20hair%20pigment%20dilution%20have%20extracutaneous%20manifestations%2C%20early%20diagnosis%20is%20vital%20in%20establishing%20multidisciplinary%20care.%22%2C%22date%22%3A%222024%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1111%5C%2Fpde.15498%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221525-1470%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A05%3A48Z%22%7D%7D%2C%7B%22key%22%3A%22JIRRVQVC%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Ju%20et%20al.%22%2C%22parsedDate%22%3A%222024-02%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BJu%20HJ%2C%20Kim%20SH%2C%20Lee%20SG%2C%20Bae%20JM.%20Eyelash%20Dyeing%20for%20Poliosis%20of%20Eyelashes%20in%20Patients%20With%20Vitiligo.%20Ann%20Dermatol.%202024%20Feb%3B36%281%29%3A56%26%23x2013%3B7.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Eyelash%20Dyeing%20for%20Poliosis%20of%20Eyelashes%20in%20Patients%20With%20Vitiligo%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Hyun%20Jeong%22%2C%22lastName%22%3A%22Ju%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Soo%20Hyung%22%2C%22lastName%22%3A%22Kim%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Seo%20Gyeong%22%2C%22lastName%22%3A%22Lee%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jung%20Min%22%2C%22lastName%22%3A%22Bae%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222024-02%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.5021%5C%2Fad.22.171%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%222005-3894%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A15%3A33Z%22%7D%7D%2C%7B%22key%22%3A%22FG6EG76C%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Lueangarun%20et%20al.%22%2C%22parsedDate%22%3A%222024-06%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BLueangarun%20S%2C%20Cho%20BS%2C%20Tempark%20T.%20Hair%20repigmentation%20of%20poliosis%20circumscripta%20in%20androgenetic%20alopecia%20patient%20treated%20with%20exosomes%20and%20fractional%20picosecond%20laser.%20J%20Cosmet%20Dermatol.%202024%20June%3B23%286%29%3A2307%26%23x2013%3B11.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Hair%20repigmentation%20of%20poliosis%20circumscripta%20in%20androgenetic%20alopecia%20patient%20treated%20with%20exosomes%20and%20fractional%20picosecond%20laser%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Suparuj%22%2C%22lastName%22%3A%22Lueangarun%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Byong%20Seung%22%2C%22lastName%22%3A%22Cho%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Therdpong%22%2C%22lastName%22%3A%22Tempark%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222024-06%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1111%5C%2Fjocd.16261%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221473-2165%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AP7EWMHX%22%5D%2C%22dateModified%22%3A%222024-09-10T16%3A11%3A04Z%22%7D%7D%5D%7D 1.
Fellman AC, Mehregan AH. Letter: Halo nevi of scalp with poliosis. Arch Dermatol. 1976 Apr;112(4):559.
1.
Herman KL, Salman K, Rose LI. White forelock in Marfan’s syndrome: an unusual association, with review of the literature. Cutis. 1991 July;48(1):82–4.
1.
Rathinam SR, Vijayalakshmi P, Namperumalsamy P, Nozik RA, Cunningham ET. Vogt-Koyanagi-Harada syndrome in children. Ocul Immunol Inflamm. 1998 Sept;6(3):155–61.
1.
Walker S, Lucke TW, Burden AD, Thomson J. Poliosis circumscripta associated with scalp naevi: a report of four cases. Br J Dermatol. 1999 June;140(6):1182–4.
1.
Elston DM, Clayton AS, Meffert JJ, McCollough ML. Migratory poliosis: A forme fruste of alopecia areata? J Am Acad Dermatol. 2000 June;42(6):1076–7.
1.
Wu JJ, Huang DB, Tyring SK. Postherpetic poliosis. Arch Dermatol. 2006 Feb;142(2):250–1.
1.
Young LC, Van Dyke GS, Lipton S, Binder SW. Poliosis overlying a nevus with blue nevus features. Dermatol Online J. 2008 Feb 28;14(2):20.
1.
Jacob SE, Blyumin M. Vitiligo-like hypopigmentation with poliosis following treatment of superficial basal cell carcinoma with imiquimod. Dermatol Surg. 2008 June;34(6):844–5.
1.
Tan C, Zhu WY. Permanent poliosis following repetitive plucking in an adolescent. J Cutan Med Surg. 2010;14(4):193–4.
1.
Bernardes TF, Bonfioli AA. Blepharitis. Semin Ophthalmol. 2010 May;25(3):79–83.
1.
Chappell JA, Chu MB, Martin K, Hurley MY. Acitretin-induced poliosis with concurrent alopecia. J Drugs Dermatol. 2012 Feb;11(2):247–9.
1.
Awad SS. Repigmentation of poliosis after epithelial grafting for vitiligo. Dermatol Surg. 2013 Mar;39(3 Pt 1):406–11.
1.
Sleiman R, Kurban M, Succaria F, Abbas O. Poliosis circumscripta: overview and underlying causes. J Am Acad Dermatol. 2013 Oct;69(4):625–33.
1.
Malik TG, Khalil M, Bhatti MM. Pityriasis alba with poliosis. J Coll Physicians Surg Pak. 2014 Feb;24(2):138–40.
1.
Feng H, Sun Y, Wang Q. Downregulation of c-Kit/MITF-M in graying hair of juvenile poliosis. Acta Derm Venereol. 2014 July;94(4):484–5.
1.
Jalalat SZ, Kelsoe JR, Cohen PR. Alopecia areata with white hair regrowth: case report and review of poliosis. Dermatol Online J. 2014 Sept 16;20(9):13030/qt1xk5b26v.
1.
Özyurt S, Çetinkaya GS. Hypertrichosis of the malar areas and poliosis of the eyelashes caused by latanoprost. Actas Dermosifiliogr. 2015;106(1):74–5.
1.
Grob A, Grekin S. Piebaldism in children. Cutis. 2016 Feb;97(2):90–2.
1.
Lee YB, Jun M, Lee WS. Alopecia areata and poliosis: A retrospective analysis of 258 cases. J Am Acad Dermatol. 2019 June;80(6):1776–8.
1.
Schollenberger MD, Stein JE, Taube JM, Lipson EJ. Poliosis Circumscripta: A Mark of Melanoma. Am J Med. 2019 Dec;132(12):1417–8.
1.
Burzi L, Parietti M, Agostini A, Marra E, Fierro MT, Ribero S, et al. Eyelashes poliosis as first sign of metastatic melanoma. J Eur Acad Dermatol Venereol. 2021 July;35(7):e459–60.
1.
Hong JY, Ahn HK, Kim S, Lee SH. Paediatric Poliosis as the Presenting Feature of Scalp Vitiligo: A Retrospective Case Series. Acta Derm Venereol. 2022 Oct 24;102:adv00800.
1.
Rodrigues G, Mendonca T. Eyelash poliosis associated with Vogt-Koyanagi Harada disease. Clin Exp Optom. 2023 Apr;106(3):338–9.
1.
Nemovi K, Jamali A, Matinpour K, Dasanu CA. Widespread vitiligo and poliosis following ipilimumab-nivolumab combination therapy. J Oncol Pharm Pract. 2023 July;29(5):1278–82.
1.
Karch JL, Davis MJ, Momtahen S, Simmons BJ. Subcutaneous Nodule With Poliosis: An Unusual Presentation of Melanoma Ex Blue Nevus. Dermatol Surg. 2023 Dec 1;49(12):1206–7.
1.
Rangu SA, Oza VS. Poliosis, hair pigment dilution, and premature graying of the hair: A diagnostic approach in pediatric patients and review of the literature. Pediatr Dermatol. 2024;41(2):197–203.
1.
Ju HJ, Kim SH, Lee SG, Bae JM. Eyelash Dyeing for Poliosis of Eyelashes in Patients With Vitiligo. Ann Dermatol. 2024 Feb;36(1):56–7.
1.
Lueangarun S, Cho BS, Tempark T. Hair repigmentation of poliosis circumscripta in androgenetic alopecia patient treated with exosomes and fractional picosecond laser. J Cosmet Dermatol. 2024 June;23(6):2307–11.