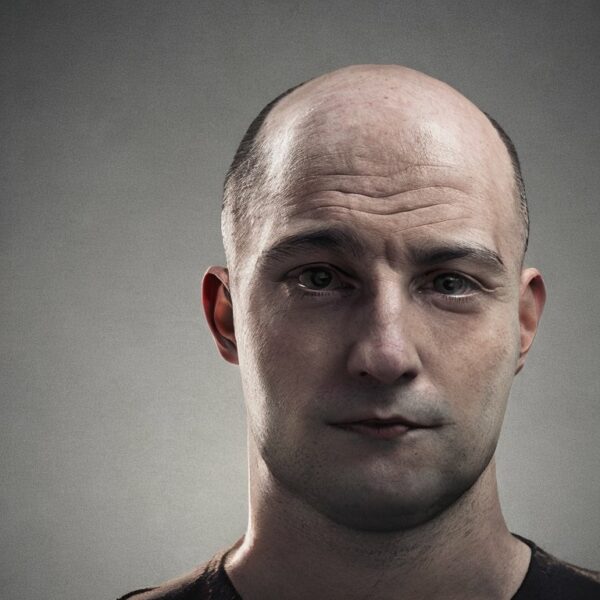
Androgenetic alopecia (AGA) is a common form of hair loss that affects both men and women. The pathology of AGA is characterized by a complex interplay of genetic, hormonal, and environmental factors that lead to progressive miniaturization of affected hair follicles on the scalp and changes in the hair growth cycle.
To look under the skin and see what happens to the hair follicles in androgenetic alopecia a punch biopsy is taken. Simply, a small metal tube with a razor sharp edge usually about 4mm in diameter is pushed into the skin at the same angle as the hair follicles. The tube acts like a paper punch and cuts a circular piece of skin out of the scalp. This sample is then sent for processing in a histology laboratory and then passed to a pathologist for analysis under a microscope.
The gradual changes that occur in the androgenetic alopecia affected scalp skin is the same whether describing male of female hair loss. A key feature of AGA is the transformation of terminal hair follicles, which produce thick, pigmented hairs, into vellus hair follicles, which produce thin, unpigmented hairs. This process, known as follicular miniaturization, results in a decrease in the density of terminal hairs and an increase in the vellus hair count. Over time, the hair growth cycle of the affected follicles becomes progressively shorter, with reduced anagen (growth) periods and increased telogen (resting) phases. This leads to a gradual increase in the number of resting hair follicles, which can reach up to 20% of the total in the early stages of AGA, compared to a normal range of up to 10% in people who don’t have hair loss.
Androgenetic alopecia does not develop in all hair follicles at the same time. Some are more quickly affected than others. When looking at a punch biopsy under the microscope neighboring hair follicles can be seen to be variably affected. Some will be normal healthy terminal hairs with an average diameter of 0.06mm, others will be miniaturized vellus hair follicles with an average diameter of 0.03mm or less. So, one parameter of androgenetic alopecia is a decrease in the density of terminal hairs and an increase in the vellus hair count. Hairs in an intermediate state somewhere in between terminal and vellus hairs will also be observed.
In addition to follicular miniaturization, AGA is associated with fibrosis, or scarring, around the affected hair follicles. Beneath the miniaturized vellus hair follicle, a fibrous tract known as a streamer or follicular stela can be observed, marking the original position of the terminal hair follicle bulb. This fibrosis is thought to contribute to the irreversible destruction of hair follicles observed in advanced stages of AGA. In addition, the arrector pili muscle (the muscle that makes your hair stand on end when it is cold) that is connected to terminal hair follicles, degenerates and is replaced with a small amount of adipose tissue.
Another important aspect of AGA pathology is the presence of an inflammatory infiltrate around the affected hair follicles. This inflammation is often more intense in AGA than in normal scalp hair follicles, with many more cells involved. The exact role of inflammation in AGA is still a subject of ongoing research, but it is thought to contribute to follicular damage and hair loss. Recent research has shed light on the complex cellular interactions involved between immune cells and the regulation of hair follicle stem cells (HFSCs), which play a crucial role in hair growth and regeneration. The role of macrophages, a type of immune cell, in sensing skin injury and promoting or inhibiting hair regeneration is a particular area of interest as macrophages can be seen to accumulate in the skin near the hair follicle stem cell regions.
Furthermore, studies highlight the role of adipose tissue and nutritional sensing in hair growth. Dermal white adipose tissue, which surrounds hair follicles, has been shown to oscillate in thickness during the hair growth cycle, and its thickness is thought to influence hair growth. In people with AGA and hair follicle miniaturization, the adipose fat layer of the skin becomes much thinner in affected areas of the scalp. Recent studies also discuss the role of sympathetic nerves in hair growth. These nerves, which surround hair follicles, are thought to relay external signals, such as light exposure, to the HFSC niche, thereby affecting hair growth. They might influence AGA through signalling changes in seasonal sunlight exposure, or high stress levels, both of which can indirectly promote hair shedding.
In conclusion, the pathology of AGA is characterized by a complex interplay of genetic, hormonal, and environmental factors that lead to changes in the hair growth cycle, follicular miniaturization, fibrosis, and inflammation in AGA affected hair follicles. Understanding these processes and their regulation can provide new insights into the prevention and treatment of AGA. Future research should focus on elucidating the complex cellular interactions involved in the hair growth cycle and the role of inflammation, fibrosis, and other factors in AGA.
Bibliography
11711645 {11711645:HNZH5C4B},{11711645:42DRMBK6},{11711645:4JSS24RT},{11711645:TXPR672U},{11711645:PJRJNE5D},{11711645:XJP897BN},{11711645:BNMQWZP3} 1 vancouver 50 date asc 125 https://www.keratin.com/wp-content/plugins/zotpress/ %7B%22status%22%3A%22success%22%2C%22updateneeded%22%3Afalse%2C%22instance%22%3Afalse%2C%22meta%22%3A%7B%22request_last%22%3A0%2C%22request_next%22%3A0%2C%22used_cache%22%3Atrue%7D%2C%22data%22%3A%5B%7B%22key%22%3A%224JSS24RT%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Whiting%22%2C%22parsedDate%22%3A%221993-05%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%201.35%3B%20%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%20style%3D%5C%22clear%3A%20left%3B%20%5C%22%3E%5Cn%20%20%20%20%3Cdiv%20class%3D%5C%22csl-left-margin%5C%22%20style%3D%5C%22float%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%5C%22%3E1.%3C%5C%2Fdiv%3E%3Cdiv%20class%3D%5C%22csl-right-inline%5C%22%20style%3D%5C%22margin%3A%200%20.4em%200%201.5em%3B%5C%22%3EWhiting%20DA.%20Diagnostic%20and%20predictive%20value%20of%20horizontal%20sections%20of%20scalp%20biopsy%20specimens%20in%20male%20pattern%20androgenetic%20alopecia.%20J%20Am%20Acad%20Dermatol.%201993%20May%3B28%285%20Pt%201%29%3A755%26%23x2013%3B63.%3C%5C%2Fdiv%3E%5Cn%20%20%20%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Diagnostic%20and%20predictive%20value%20of%20horizontal%20sections%20of%20scalp%20biopsy%20specimens%20in%20male%20pattern%20androgenetic%20alopecia%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22D.%20A.%22%2C%22lastName%22%3A%22Whiting%22%7D%5D%2C%22abstractNote%22%3A%22BACKGROUND%3A%20Vertical%20sections%20of%20small%20scalp%20biopsy%20specimens%20are%20often%20inadequate%20for%20the%20diagnosis%20of%20male%20pattern%20androgenetic%20alopecia%20%28MPAA%29.%20Quantitative%20analysis%20of%20follicular%20structures%20in%20horizontal%20sections%20can%20provide%20more%20information.%5CnOBJECTIVES%3A%20Our%20purpose%20was%20to%20establish%20better%20diagnostic%20criteria%20by%20comparing%20horizontal%20and%20vertical%20sections%20of%20scalp%20biopsy%20specimens%20from%20MPAA%20and%20normal%20control%20subjects%20and%20to%20determine%20the%20predictive%20value%20of%20horizontal%20sections%2C%20by%20relating%20counts%20of%20follicular%20structures%20in%20MPAA%20to%20subsequent%20hair%20regrowth%20from%20topical%20minoxidil%20therapy.%5CnMETHODS%3A%20Paired%204%20mm%20punch%20biopsy%20specimens%20were%20taken%20from%2022%20normal%20control%20subjects%20and%20106%20patients%20with%20MPAA%2C%20for%20horizontal%20and%20vertical%20sectioning.%20In%20horizontal%20sections%2C%20hair%20bulbs%2C%20terminal%20anagen%2C%20catagen%20and%20telogen%20hairs%2C%20telogen%20germinal%20units%2C%20and%20vellus%20hairs%20were%20counted%2C%20as%20were%20follicular%20units%20and%20stelae.%5CnRESULTS%3A%20The%20diagnosis%20of%20MPAA%20was%20confirmed%20by%20finding%20decreased%20terminal%20hairs%20and%20increased%20stelae%20and%20vellus%20hairs.%20The%20average%20horizontal%20section%20contained%2022%20terminal%20and%2013%20vellus%20hairs%2C%20a%201.7%3A1%20ratio.%20Changes%20compatible%20with%20MPAA%20were%20found%20in%20most%20vertical%20and%20horizontal%20sections%2C%20but%20horizontal%20sections%20were%20required%20for%20follicular%20counts%20and%20showed%20terminal%3Avellus%20hair%20ratios%20diagnostic%20of%20MPAA%20in%2067%25%20of%20cases.%20Of%2044%20patients%20treated%20with%20topical%20minoxidil%2C%20five%20with%20less%20than%202%20follicular%20structures%5C%2Fmm2%20showed%20no%20hair%20regrowth%2C%2032%20with%202%20to%204%20follicular%20structures%5C%2Fmm2%20showed%20regrowth%20in%2072%25%2C%20and%20seven%20with%20more%20than%204%20follicular%20structures%5C%2Fmm2%20showed%20regrowth%20in%2086%25%20of%20cases.%20In%20MPAA%20with%20no%20significant%20inflammation%2C%20regrowth%20occurred%20in%2077%25%20of%20cases%2C%20versus%2055%25%20in%20cases%20with%20significant%20inflammation.%5CnCONCLUSION%3A%20Horizontal%20sections%20of%20scalp%20biopsy%20specimens%20in%20MPAA%20provide%20more%20diagnostic%20information%20than%20vertical%20sections%20and%20appear%20to%20have%20a%20predictive%20value%20for%20hair%20regrowth.%22%2C%22date%22%3A%221993-05%22%2C%22language%22%3A%22eng%22%2C%22DOI%22%3A%2210.1016%5C%2F0190-9622%2893%2970106-4%22%2C%22ISSN%22%3A%220190-9622%22%2C%22url%22%3A%22%22%2C%22collections%22%3A%5B%22J8CSTEXG%22%5D%2C%22dateModified%22%3A%222023-05-19T15%3A32%3A13Z%22%7D%7D%2C%7B%22key%22%3A%22PJRJNE5D%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22de%20Lacharri%5Cu00e8re%20et%20al.%22%2C%22parsedDate%22%3A%222001-05%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%201.35%3B%20%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%20style%3D%5C%22clear%3A%20left%3B%20%5C%22%3E%5Cn%20%20%20%20%3Cdiv%20class%3D%5C%22csl-left-margin%5C%22%20style%3D%5C%22float%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%5C%22%3E1.%3C%5C%2Fdiv%3E%3Cdiv%20class%3D%5C%22csl-right-inline%5C%22%20style%3D%5C%22margin%3A%200%20.4em%200%201.5em%3B%5C%22%3Ede%20Lacharri%26%23xE8%3Bre%20O%2C%20Deloche%20C%2C%20Misciali%20C%2C%20Piraccini%20BM%2C%20Vincenzi%20C%2C%20Bastien%20P%2C%20et%20al.%20Hair%20diameter%20diversity%3A%20a%20clinical%20sign%20reflecting%20the%20follicle%20miniaturization.%20Arch%20Dermatol.%202001%20May%3B137%285%29%3A641%26%23x2013%3B6.%3C%5C%2Fdiv%3E%5Cn%20%20%20%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Hair%20diameter%20diversity%3A%20a%20clinical%20sign%20reflecting%20the%20follicle%20miniaturization%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22O.%22%2C%22lastName%22%3A%22de%20Lacharri%5Cu00e8re%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22C.%22%2C%22lastName%22%3A%22Deloche%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22C.%22%2C%22lastName%22%3A%22Misciali%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22B.%20M.%22%2C%22lastName%22%3A%22Piraccini%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22C.%22%2C%22lastName%22%3A%22Vincenzi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22P.%22%2C%22lastName%22%3A%22Bastien%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22I.%22%2C%22lastName%22%3A%22Tardy%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22B.%20A.%22%2C%22lastName%22%3A%22Bernard%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22A.%22%2C%22lastName%22%3A%22Tosti%22%7D%5D%2C%22abstractNote%22%3A%22BACKGROUND%3A%20The%20degree%20of%20androgenetic%20alopecia%20is%20generally%20evaluated%20either%20by%20global%20clinical%20scales%20or%20time-consuming%20methods%20like%20phototrichogram%20or%20histological%20studies.%20We%20describe%20a%20new%20clinical%20and%20reliable%20scoring%20method%20based%20on%20hair%20diameter%20diversity.%5CnOBSERVATIONS%3A%20%281%29%20The%20clinical%20macroscopic%20scoring%20we%20propose%20for%20hair%20density%20was%20significantly%20correlated%20with%20Hamilton%20classification%20and%20with%20histological%20hair%20density.%20%282%29%20Diversity%20in%20hair%20diameter%20was%20the%20main%20and%20most%20accurate%20clinical%20parameter%20linked%20to%20follicle%20miniaturization.%20%28C%29%20The%20anagen-telogen%20ratio%20decreased%20in%20parallel%20with%20the%20decrease%20in%20clinical%20hair%20density%20score.%5CnCONCLUSIONS%3A%20Considering%20that%20hair%20follicle%20miniaturization%20is%20the%20key%20point%20during%20androgenic%20alopecia%20onset%20and%20development%2C%20diversity%20in%20hair%20diameter%20represents%20an%20important%20feature%20to%20consider%20as%20an%20accurate%20clinical%20sign%20reflecting%20hair%20follicle%20miniaturization.%20Moreover%2C%20diversity%20in%20hair%20diameter%20seems%20to%20be%20an%20easily%20accessible%20and%20reliable%20parameter%20that%20should%20be%20taken%20into%20consideration%20for%20further%20characterization%20of%20hair%20disorders.%20By%20itself%2C%20we%20believe%20that%20this%20clinical%20feature%20constitutes%20a%20new%20tool%20of%20substantial%20help%20for%20the%20diagnosis%20and%20management%20of%20androgenic%20alopecia.%22%2C%22date%22%3A%222001-05%22%2C%22language%22%3A%22eng%22%2C%22DOI%22%3A%22%22%2C%22ISSN%22%3A%220003-987X%22%2C%22url%22%3A%22%22%2C%22collections%22%3A%5B%22J8CSTEXG%22%5D%2C%22dateModified%22%3A%222023-05-19T15%3A32%3A45Z%22%7D%7D%2C%7B%22key%22%3A%22XJP897BN%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Deloche%20et%20al.%22%2C%22parsedDate%22%3A%222004-03%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%201.35%3B%20%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%20style%3D%5C%22clear%3A%20left%3B%20%5C%22%3E%5Cn%20%20%20%20%3Cdiv%20class%3D%5C%22csl-left-margin%5C%22%20style%3D%5C%22float%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%5C%22%3E1.%3C%5C%2Fdiv%3E%3Cdiv%20class%3D%5C%22csl-right-inline%5C%22%20style%3D%5C%22margin%3A%200%20.4em%200%201.5em%3B%5C%22%3EDeloche%20C%2C%20de%20Lacharri%26%23xE8%3Bre%20O%2C%20Misciali%20C%2C%20Piraccini%20BM%2C%20Vincenzi%20C%2C%20Bastien%20P%2C%20et%20al.%20Histological%20features%20of%20peripilar%20signs%20associated%20with%20androgenetic%20alopecia.%20Arch%20Dermatol%20Res.%202004%20Mar%3B295%2810%29%3A422%26%23x2013%3B8.%3C%5C%2Fdiv%3E%5Cn%20%20%20%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Histological%20features%20of%20peripilar%20signs%20associated%20with%20androgenetic%20alopecia%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Claire%22%2C%22lastName%22%3A%22Deloche%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Olivier%22%2C%22lastName%22%3A%22de%20Lacharri%5Cu00e8re%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Cosimo%22%2C%22lastName%22%3A%22Misciali%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Bianca%20Maria%22%2C%22lastName%22%3A%22Piraccini%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Colombina%22%2C%22lastName%22%3A%22Vincenzi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Philippe%22%2C%22lastName%22%3A%22Bastien%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Isabelle%22%2C%22lastName%22%3A%22Tardy%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Bruno%20A.%22%2C%22lastName%22%3A%22Bernard%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Antonella%22%2C%22lastName%22%3A%22Tosti%22%7D%5D%2C%22abstractNote%22%3A%22BACKGROUND%3A%20A%20study%20of%20the%20scalp%20in%20a%20large%20cohort%20of%20volunteers%20with%20androgenetic%20alopecia%20using%20macrophotographs%20showed%20the%20presence%20of%20peripilar%20signs%20%28PPS%29%20around%20the%20hair%20ostia.%5CnOBJECTIVE%3A%20The%20aim%20of%20the%20present%20study%20was%20to%20establish%20the%20histopathological%20features%20related%20to%20PPS.%5CnDESIGN%3A%20Prospective%20clinicopathological%20study.%20SETTING.%20Department%20of%20Dermatology%2C%20University%20Hospital%20of%20Bologna.%5CnPATIENTS%3A%20A%20group%20of%2040%20patients%20%2821%20males%20and%2019%20females%29%20participated%20in%20the%20study.%20Macrophotographs%20of%20the%20scalp%20were%20taken%20using%20a%20Dermaphot%20camera%20and%20PPS%20were%20scored%20using%20a%20three-point%20scale.%20Hair%20density%20and%20PPS%20were%20clinically%20scored%20according%20to%20reference%20scales.%20Two%20punch%20biopsies%20from%20the%20photographed%20area%20were%20obtained%20from%20each%20subject%20and%20histological%20analysis%20was%20performed%20on%20vertical%20and%20horizontal%20sections.%5CnOBSERVATIONS%3A%20Clinical%20parameters%20indicated%20that%20PPS%20were%20already%20detectable%20on%20scalp%20with%20high%20hair%20density.%20Moreover%2C%20in%20patients%20with%20high%20hair%20density%20%28score%20%3E4%29%2C%20a%20significant%20relationship%20was%20found%20between%20the%20PPS%20score%20and%20the%20global%20score%20for%20perifollicular%20infiltrates.%20Thus%20PPS%20are%20linked%20to%20superficial%20perifollicular%20lymphocytic%20infiltrates%20in%20early%20androgenetic%20alopecia.%5CnCONCLUSIONS%3A%20PPS%20could%20be%20the%20clinical%20signs%20reflecting%20the%20presence%20of%20perifollicular%20infiltrates.%22%2C%22date%22%3A%222004-03%22%2C%22language%22%3A%22eng%22%2C%22DOI%22%3A%2210.1007%5C%2Fs00403-003-0447-y%22%2C%22ISSN%22%3A%220340-3696%22%2C%22url%22%3A%22%22%2C%22collections%22%3A%5B%22J8CSTEXG%22%5D%2C%22dateModified%22%3A%222023-05-19T15%3A29%3A54Z%22%7D%7D%2C%7B%22key%22%3A%22HNZH5C4B%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22El-Domyati%20et%20al.%22%2C%22parsedDate%22%3A%222009-06%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%201.35%3B%20%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%20style%3D%5C%22clear%3A%20left%3B%20%5C%22%3E%5Cn%20%20%20%20%3Cdiv%20class%3D%5C%22csl-left-margin%5C%22%20style%3D%5C%22float%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%5C%22%3E1.%3C%5C%2Fdiv%3E%3Cdiv%20class%3D%5C%22csl-right-inline%5C%22%20style%3D%5C%22margin%3A%200%20.4em%200%201.5em%3B%5C%22%3EEl-Domyati%20M%2C%20Attia%20S%2C%20Saleh%20F%2C%20Abdel-Wahab%20H.%20Androgenetic%20alopecia%20in%20males%3A%20a%20histopathological%20and%20ultrastructural%20study.%20J%20Cosmet%20Dermatol.%202009%20Jun%3B8%282%29%3A83%26%23x2013%3B91.%3C%5C%2Fdiv%3E%5Cn%20%20%20%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Androgenetic%20alopecia%20in%20males%3A%20a%20histopathological%20and%20ultrastructural%20study%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Moetaz%22%2C%22lastName%22%3A%22El-Domyati%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Sameh%22%2C%22lastName%22%3A%22Attia%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Fatma%22%2C%22lastName%22%3A%22Saleh%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Hossam%22%2C%22lastName%22%3A%22Abdel-Wahab%22%7D%5D%2C%22abstractNote%22%3A%22BACKGROUND%3A%20Androgenetic%20alopecia%20is%20a%20common%20cosmetic%20hair%20disorder%2C%20resulting%20from%20interplay%20of%20genetic%2C%20endocrine%2C%20and%20aging%20factors%20leading%20to%20a%20patterned%20follicular%20miniaturization.%20Microinflammation%20seems%20to%20be%20a%20potential%20active%20player%20in%20this%20process.%5CnAIMS%3A%20To%20study%20the%20histopathological%20and%20ultrastructural%20changes%20occurring%20in%20male%20androgenetic%20alopecia%20%28AGA%29.%20Patients%5C%2Fmethods%20Fifty-five%20subjects%20were%20included%20in%20this%20study%20%2840%20with%20AGA%20and%2015%20as%20normal%20age-matched%20controls%29.%20Skin%20biopsies%20from%20frontal%20bald%20area%20and%20occipital%20hairy%20area%20were%20subjected%20to%20histopathological%20examination%2C%20immunohistochemical%20staining%20for%20collagen%20I%20and%20ultrastructural%20study.%5CnRESULTS%3A%20The%20frontal%20bald%20area%20of%20patients%20showed%20highly%20significant%20increase%20in%20telogen%20hairs%20and%20decrease%20in%20anagen%5C%2Ftelogen%20ratio%20and%20terminal%5C%2Fvellus%20hair%20ratio%20%28P%20%3C%200.001%29.%20Perifollicular%20inflammation%20was%20almost%20a%20constant%20feature%20in%20early%20cases%20and%20showed%20a%20significant%20inverse%20correlation%20with%20perifollicular%20fibrosis%20%28P%20%3D%200.048%29%2C%20which%20was%20more%20marked%20with%20thickening%20of%20the%20follicular%20sheath%20in%20advanced%20cases.%5CnCONCLUSION%3A%20Follicular%20microinflammation%20plays%20an%20integral%20role%20in%20the%20pathogenesis%20of%20AGA%20in%20early%20cases.%20Over%20time%2C%20thickening%20of%20perifollicular%20sheath%20takes%20place%20due%20to%20increased%20deposition%20of%20collagen%2C%20resulting%20in%20marked%20perifollicular%20fibrosis%2C%20and%20sometimes%20ends%20by%20complete%20destruction%20of%20the%20affected%20follicles%20in%20advanced%20cases.%22%2C%22date%22%3A%222009-06%22%2C%22language%22%3A%22eng%22%2C%22DOI%22%3A%2210.1111%5C%2Fj.1473-2165.2009.00439.x%22%2C%22ISSN%22%3A%221473-2165%22%2C%22url%22%3A%22%22%2C%22collections%22%3A%5B%22J8CSTEXG%22%5D%2C%22dateModified%22%3A%222023-05-19T15%3A31%3A23Z%22%7D%7D%2C%7B%22key%22%3A%22TXPR672U%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Aslani%20et%20al.%22%2C%22parsedDate%22%3A%222009-07%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%201.35%3B%20%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%20style%3D%5C%22clear%3A%20left%3B%20%5C%22%3E%5Cn%20%20%20%20%3Cdiv%20class%3D%5C%22csl-left-margin%5C%22%20style%3D%5C%22float%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%5C%22%3E1.%3C%5C%2Fdiv%3E%3Cdiv%20class%3D%5C%22csl-right-inline%5C%22%20style%3D%5C%22margin%3A%200%20.4em%200%201.5em%3B%5C%22%3EAslani%20FS%2C%20Dastgheib%20L%2C%20Banihashemi%20BM.%20Hair%20counts%20in%20scalp%20biopsy%20of%20males%20and%20females%20with%20androgenetic%20alopecia%20compared%20with%20normal%20subjects.%20J%20Cutan%20Pathol.%202009%20Jul%3B36%287%29%3A734%26%23x2013%3B9.%3C%5C%2Fdiv%3E%5Cn%20%20%20%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Hair%20counts%20in%20scalp%20biopsy%20of%20males%20and%20females%20with%20androgenetic%20alopecia%20compared%20with%20normal%20subjects%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Fatemeh%20Sari%22%2C%22lastName%22%3A%22Aslani%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ladan%22%2C%22lastName%22%3A%22Dastgheib%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Bibi%20Maryam%22%2C%22lastName%22%3A%22Banihashemi%22%7D%5D%2C%22abstractNote%22%3A%22BACKGROUND%3A%20Hair%20counts%20were%20studied%20in%20scalp%20biopsy%20specimens%20of%20androgenetic%20alopecia%20%28AGA%29%20in%20male%20and%20female%20patients.%20We%20also%20assessed%20the%20normal%20value%20of%20hair%20count%20in%20scalp%20biopsy%20specimen%20from%20Iranians%20and%20compared%20with%20published%20data.%5CnMETHODS%3A%20Thirty%20subjects%20with%20clinically%20normal%20scalps%2C%2025%20male%20and%2028%20female%20patients%20with%20AGA%20were%20studied.%20Vertical%20and%20horizontal%20sections%20of%204-mm%20punch%20biopsy%20specimens%20were%20examined%20at%20various%20levels%20from%20the%20papillary%20dermis%20to%20the%20subcutis.%20Hair%20counts%20of%20total%2C%20terminal%2C%20vellus%2C%20anagen%20and%20telogen%20hairs%20were%20obtained%20by%20ocular%20micrometer.%5CnRESULTS%3A%20Hair%20counts%20were%20not%20significantly%20different%20from%20published%20data%20in%20American%20Whites%20but%20significantly%20higher%20in%20Iranians%20compared%20with%20Koreans%20%28p%20%3C%200.001%29.%20There%20was%20no%20significant%20difference%20between%20male%20and%20female%20patients%20with%20AGA.%20Perifollicular%20inflammation%20was%20lower%20in%20both%20the%20normal%20subjects%20and%20the%20patients%20compared%20with%20other%20studies.%5CnCONCLUSION%3A%20In%20AGA%20patients%2C%20total%20and%20vellus%20hairs%20were%20lower%20and%20terminal%20to%20vellus%20%28T%3AV%29%20ratio%20was%20higher%20than%20the%20results%20of%20previous%20studies%20in%20Whites%20%28p%20%3C%2000.1%29.%20T%3AV%20ratio%20of%20control%20group%20was%20significantly%20higher%20in%20this%20study%20compared%20with%20previous%20published%20data.%20Perhaps%20the%20higher%20ratio%20than%20the%20reported%20data%20could%20means%20the%20onset%20of%20miniaturization.%22%2C%22date%22%3A%222009-07%22%2C%22language%22%3A%22eng%22%2C%22DOI%22%3A%2210.1111%5C%2Fj.1600-0560.2008.01149.x%22%2C%22ISSN%22%3A%221600-0560%22%2C%22url%22%3A%22%22%2C%22collections%22%3A%5B%22J8CSTEXG%22%5D%2C%22dateModified%22%3A%222023-05-19T15%3A31%3A53Z%22%7D%7D%2C%7B%22key%22%3A%22BNMQWZP3%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Ekmekci%20et%20al.%22%2C%22parsedDate%22%3A%222010-03%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%201.35%3B%20%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%20style%3D%5C%22clear%3A%20left%3B%20%5C%22%3E%5Cn%20%20%20%20%3Cdiv%20class%3D%5C%22csl-left-margin%5C%22%20style%3D%5C%22float%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%5C%22%3E1.%3C%5C%2Fdiv%3E%3Cdiv%20class%3D%5C%22csl-right-inline%5C%22%20style%3D%5C%22margin%3A%200%20.4em%200%201.5em%3B%5C%22%3EEkmekci%20TR%2C%20Sakiz%20D%2C%20Koslu%20A.%20Occipital%20involvement%20in%20female%20pattern%20hair%20loss%3A%20histopathological%20evidences.%20J%20Eur%20Acad%20Dermatol%20Venereol.%202010%20Mar%3B24%283%29%3A299%26%23x2013%3B301.%3C%5C%2Fdiv%3E%5Cn%20%20%20%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Occipital%20involvement%20in%20female%20pattern%20hair%20loss%3A%20histopathological%20evidences%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22T.%20R.%22%2C%22lastName%22%3A%22Ekmekci%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22D.%22%2C%22lastName%22%3A%22Sakiz%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22A.%22%2C%22lastName%22%3A%22Koslu%22%7D%5D%2C%22abstractNote%22%3A%22BACKGROUND%3A%20Female%20pattern%20hair%20loss%20%28FPHL%29%20is%20characterized%20by%20diffuse%20thinning%20of%20hair%20in%20the%20frontal%20and%20parietal%20areas%20of%20the%20scalp%2C%20and%20preservation%20of%20the%20frontal%20hairline%20is%20the%20norm.%20Hair%20on%20the%20occipital%20scalp%20is%20thought%20to%20be%20preserved.%5CnOBJECTIVE%3A%20To%20investigate%20whether%20the%20occipital%20area%20is%20involved%20in%20FPHL%20or%20whether%20there%20is%20a%20diffuse%20type%20of%20FPHL.%5CnMETHODS%3A%20Forty%20female%20patients%20who%20had%20complained%20about%20hair%20loss%20for%20more%20than%20a%20year%20and%20were%20diagnosed%20with%20FPHL%20according%20to%20the%20Ludwig%20classification%20were%20included.%20Two%20punch%20biopsies%20from%20both%20the%20midscalp%20and%20the%20occiput%20were%20taken.%20Histological%20sections%20were%20prepared%20horizontally%20and%20stained%20with%20haematoxylin%20and%20eosin.%20Terminal%20follicles%2C%20vellus%20like%20follicles%2C%20anagen%2C%20telogen%2C%20catagen%20follicles%2C%20hair%20bulbs%20and%20telogen%20germinal%20units%20were%20counted%20in%20two%20sections%20of%20the%20upper%20dermis%20and%20the%20dermal-subcutaneous%20junction.%20If%20the%20terminal%5C%2Fvellus%20ratio%20was%20lower%20than%204%3A1%2C%20the%20diagnosis%20of%20androgenetic%20alopecia%20%28AGA%29%20was%20made.%20When%20the%20ratio%20was%20between%20four%20and%20seven%20to%20one%2C%20AGA%20was%20suspected.%5CnRESULTS%3A%20While%2029%20of%2040%20patients%20%2872.5%25%29%20had%20findings%20consistent%20with%20AGA%20on%20the%20midscalp%2C%2011%20of%2040%20%2827.5%25%29%20displayed%20signs%20of%20suspected%20AGA.%20Ten%20of%2040%20patients%20%2825%25%29%20had%20AGA%20involving%20the%20occiput.%5CnCONCLUSION%3A%20The%20involvement%20of%20the%20occipital%20scalp%20is%20significant%20in%20FPHL.%20In%20some%20patients%2C%20this%20situation%20may%20be%20so%20apparent%20that%20clinically%20visible%20alopecia%20is%20seen.%20However%2C%20in%20other%20patients%2C%20it%20may%20also%20present%20only%20as%20thinning.%22%2C%22date%22%3A%222010-03%22%2C%22language%22%3A%22eng%22%2C%22DOI%22%3A%2210.1111%5C%2Fj.1468-3083.2009.03411.x%22%2C%22ISSN%22%3A%221468-3083%22%2C%22url%22%3A%22%22%2C%22collections%22%3A%5B%22J8CSTEXG%22%5D%2C%22dateModified%22%3A%222023-05-19T15%3A33%3A28Z%22%7D%7D%2C%7B%22key%22%3A%2242DRMBK6%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Torkamani%20et%20al.%22%2C%22parsedDate%22%3A%222014-06%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%3Cdiv%20class%3D%5C%22csl-bib-body%5C%22%20style%3D%5C%22line-height%3A%201.35%3B%20%5C%22%3E%5Cn%20%20%3Cdiv%20class%3D%5C%22csl-entry%5C%22%20style%3D%5C%22clear%3A%20left%3B%20%5C%22%3E%5Cn%20%20%20%20%3Cdiv%20class%3D%5C%22csl-left-margin%5C%22%20style%3D%5C%22float%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%5C%22%3E1.%3C%5C%2Fdiv%3E%3Cdiv%20class%3D%5C%22csl-right-inline%5C%22%20style%3D%5C%22margin%3A%200%20.4em%200%201.5em%3B%5C%22%3ETorkamani%20N%2C%20Rufaut%20NW%2C%20Jones%20L%2C%20Sinclair%20R.%20Destruction%20of%20the%20arrector%20pili%20muscle%20and%20fat%20infiltration%20in%20androgenic%20alopecia.%20Br%20J%20Dermatol.%202014%20Jun%3B170%286%29%3A1291%26%23x2013%3B8.%3C%5C%2Fdiv%3E%5Cn%20%20%20%3C%5C%2Fdiv%3E%5Cn%3C%5C%2Fdiv%3E%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Destruction%20of%20the%20arrector%20pili%20muscle%20and%20fat%20infiltration%20in%20androgenic%20alopecia%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22N.%22%2C%22lastName%22%3A%22Torkamani%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22N.%20W.%22%2C%22lastName%22%3A%22Rufaut%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22L.%22%2C%22lastName%22%3A%22Jones%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22R.%22%2C%22lastName%22%3A%22Sinclair%22%7D%5D%2C%22abstractNote%22%3A%22BACKGROUND%3A%20Androgenic%20alopecia%20%28AGA%29%20is%20the%20most%20common%20hair%20loss%20condition%20in%20men%20and%20women.%20Hair%20loss%20is%20caused%20by%20follicle%20miniaturization%2C%20which%20is%20largely%20irreversible%20beyond%20a%20certain%20degree%20of%20follicular%20regression.%20In%20contrast%2C%20hair%20loss%20in%20telogen%20effluvium%20%28TE%29%20is%20readily%20reversible.%20The%20arrector%20pili%20muscle%20%28APM%29%20connects%20the%20follicle%20to%20the%20surrounding%20skin.%5CnOBJECTIVES%3A%20To%20compare%20histopathological%20features%20of%20the%20APM%20in%20AGA%20and%20TE.%5CnMETHODS%3A%20Archival%20blocks%20of%204-mm%20scalp%20punch%20biopsies%20from%20eight%20patients%20with%20AGA%20and%20five%20with%20TE%20were%20obtained.%20New%204-mm%20biopsies%20from%20five%20normal%20cases%20were%20used%20as%20controls.%20Serial%207-%5Cu03bcm%20sections%20were%20stained%20with%20a%20modified%20Masson%27s%20trichrome%20stain.%20%27Reconstruct%27%20software%20was%20used%20to%20construct%20and%20evaluate%20three-dimensional%20images%20of%20the%20follicle%20and%20APM.%5CnRESULTS%3A%20The%20APM%20degenerated%20and%20was%20replaced%20by%20adipose%20tissue%20in%20all%20AGA%20specimens.%20Remnants%20of%20the%20APM%20remained%20attached%20to%20the%20hair%20follicle.%20There%20was%20no%20fat%20in%20the%20normal%20skin%20specimens.%20Fat%20was%20seen%20in%20two%20of%20five%20TE%20specimens%20but%20could%20be%20attributed%20to%20these%20patients%20also%20showing%20evidence%20of%20AGA.%20Quantitative%20analysis%20showed%20that%20muscle%20volume%20decreased%20and%20fat%20volume%20increased%20significantly%20%28P%5Cu00a0%3C%5Cu00a00%5Cu00b705%29%20in%20AGA%20compared%20with%20controls.%5CnCONCLUSIONS%3A%20APM%20degeneration%20and%20replacement%20with%20fat%20in%20AGA%20has%20not%20previously%20been%20described.%20The%20underlying%20mechanism%20remains%20to%20be%20determined.%20However%2C%20we%20speculate%20that%20this%20phenomenon%20might%20be%20related%20to%20depletion%20of%20stem%20or%20progenitor%20cells%20from%20the%20follicle%20mesenchyme%2C%20explaining%20why%20AGA%20is%20treatment%20resistant.%22%2C%22date%22%3A%222014-06%22%2C%22language%22%3A%22eng%22%2C%22DOI%22%3A%2210.1111%5C%2Fbjd.12921%22%2C%22ISSN%22%3A%221365-2133%22%2C%22url%22%3A%22%22%2C%22collections%22%3A%5B%22J8CSTEXG%22%5D%2C%22dateModified%22%3A%222023-05-19T15%3A41%3A22Z%22%7D%7D%5D%7D 1.
Whiting DA. Diagnostic and predictive value of horizontal sections of scalp biopsy specimens in male pattern androgenetic alopecia. J Am Acad Dermatol. 1993 May;28(5 Pt 1):755–63.
1.
de Lacharrière O, Deloche C, Misciali C, Piraccini BM, Vincenzi C, Bastien P, et al. Hair diameter diversity: a clinical sign reflecting the follicle miniaturization. Arch Dermatol. 2001 May;137(5):641–6.
1.
Deloche C, de Lacharrière O, Misciali C, Piraccini BM, Vincenzi C, Bastien P, et al. Histological features of peripilar signs associated with androgenetic alopecia. Arch Dermatol Res. 2004 Mar;295(10):422–8.
1.
El-Domyati M, Attia S, Saleh F, Abdel-Wahab H. Androgenetic alopecia in males: a histopathological and ultrastructural study. J Cosmet Dermatol. 2009 Jun;8(2):83–91.
1.
Aslani FS, Dastgheib L, Banihashemi BM. Hair counts in scalp biopsy of males and females with androgenetic alopecia compared with normal subjects. J Cutan Pathol. 2009 Jul;36(7):734–9.
1.
Ekmekci TR, Sakiz D, Koslu A. Occipital involvement in female pattern hair loss: histopathological evidences. J Eur Acad Dermatol Venereol. 2010 Mar;24(3):299–301.
1.
Torkamani N, Rufaut NW, Jones L, Sinclair R. Destruction of the arrector pili muscle and fat infiltration in androgenic alopecia. Br J Dermatol. 2014 Jun;170(6):1291–8.