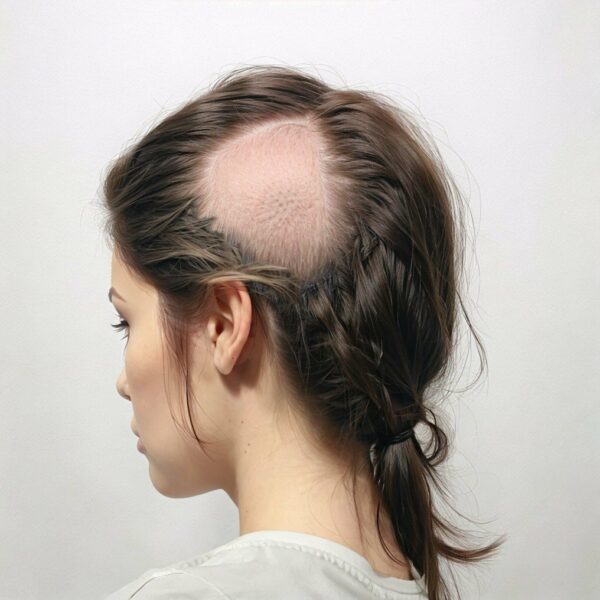
Alopecia areata (AA) is a complex autoimmune condition characterized by the sudden loss of hair, often in well-defined circular areas, while adjacent hair follicles remain unaffected. This phenomenon presents a fascinating dichotomy in disease manifestation, underlying the intricate interplay between genetic predispositions, immune system dysregulation, and the unique microenvironments of hair follicles. To understand why AA affects only specific areas, we need to delve into the pathophysiology of the disease, the role of the immune system in targeting hair follicles, and the potential factors that make certain hair follicles more susceptible than others.
The Pathophysiology of Alopecia Areata: AA is primarily an autoimmune disorder, where the body’s immune system mistakenly attacks the hair follicles, causing hair loss. Genetic predisposition plays a significant role in AA, at least for some who can point to a family history of the condition. It is possible that this genetic susceptibility may also influence which hair follicles are targeted by the immune system. This attack is largely mediated by T lymphocytes, a type of white blood cell involved in immune responses. The disease is characterized by the presence of autoreactive T cells around the affected hair follicles, leading to inflammation and the subsequent cessation of hair growth. However, often this process does not uniformly affect all hair follicles across the scalp or body, leading to the patchy hair loss typical of AA.
Immune Privilege of Hair Follicles: One key concept in understanding the localized effect of AA is the notion of “immune privilege” (IP). Hair follicles, particularly in the anagen (growth) phase, are considered immune-privileged sites. This means they are normally protected from immune system surveillance by various mechanisms, including the expression of immunosuppressive molecules and the physical barrier of the hair follicle sheath. This immune privilege is thought to prevent the immune system from attacking the rapidly dividing cells in the hair follicle, which could otherwise be mistaken for foreign or malignant cells.
Local Collapse of Immune Privilege: In individuals with AA, the immune privilege of certain hair follicles is breached or collapses, leading to an autoimmune attack. The reasons for the collapse of IP in specific follicles while others remain unaffected are poorly understood, but are believed to involve a combination of local immune responses and environmental triggers. For example, a small injury to an area of the scalp, such as bumping the head and causing a bruise, may lead to some mild damage to a few hair follicles in the bumped area. Wound healing involves the immune system, so immune cells infiltrate into the area to be healed. However, these cells may become “confused” and instead of healing the injury, they may signal an inflammatory response instead that leads to the start of a hair loss patch. Other possible local triggers to initiate onset of AA have been suggested to include changes to the local biome – perhaps some more pathogenic bacteria gets inside a few hair follicles and initiates an immune response that leads to AA. Or an overly tight ponytail might lead to some traction alopecia in a few follicles that then triggers onset.
Hair Follicle Heterogeneity: Another factor contributing to the patchy manifestation of AA is the heterogeneity of hair follicles themselves. We know some follicles are bigger than others, some grow hair faster than others, so there are differences between hair follicles on the scalp and this may make some follicles more susceptible to AA inflammation than others. Some hair follicles can be in different phases of the hair growth cycle (anagen, catagen, telogen). Follicles in the anagen phase are more likely to be affected by AA due to their higher metabolic activity and increased expression of proteins related to hair growth that seem to make them more susceptible to immune attack. Conversely, follicles in the telogen (resting) phase are less active and might temporarily escape immune surveillance, leading to the preservation of hair in areas adjacent to the lesions.
The Role of Cytokines and the Ripple Effect: The localized nature of AA is further influenced by the role of cytokines and chemokines, signaling molecules that mediate inflammation and immune responses. These molecules can create an environment that either promotes or inhibits the immune attack on hair follicles. The differential expression of these molecules around affected and unaffected follicles might explain why only certain areas are targeted. For example, the overexpression of certain cytokines, such as interleukin-15 (IL-15), has been associated with the recruitment of autoreactive T cells to the follicle, promoting hair loss. This knowledge has led to a hypothesis of alopecia areata patch expansion that can best be described as a “ripple effect”. For example, one or two hair follicles may become damaged and an immune response occurs involving immune cells and production of cytokines around the follicles. These cytokine diffuse through the skin and spread to adjacent hair follicles. These follicles then send out danger signals which attracts more immune cells to these follicles. The process continues like the ripples spreading out when a stone is thrown into a lake of water.
Stress and Local Scalp Effects: While stress has been linked to the onset of alopecia areata for many years, a more recent study has suggested that patches of alopecia areata are more likely to occur close to important scalp nerve channels. Patches of alopecia areata most commonly present on the occiput (back of the scalp) of the scalp in both female and male patients. Cervical spine nerves C3 and C2 supply sensory innervation and the occipital artery supplies blood to this area. From other research we know that nerve cells under stress produce stress hormones and neuropeptides (which are another category of chemokine signalling molecules). It has been suggested that the scalp skin nerves, during stress and other events, might start secreting stress hormones and neuropeptides. These might then diffuse out from the nerves into the skin and affect the hair follicles in the area. Other research has shown the neuropeptides, particularly one called “substance P”, can reduce the immune privilege function of hair follicles. As a result, these hair follicles may be more susceptible to inflammation and this could explain why alopecia areata most commonly begins at the back of the scalp.
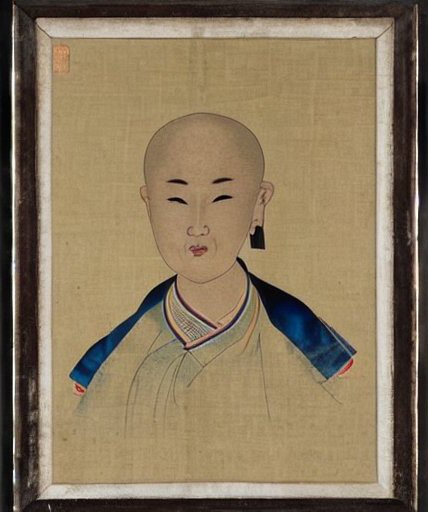
Pigmented Hair versus White Hair: It has been suggested that pigmented hair producing follicles are more susceptible to AA compared to white hair. When a lesion develops in someone with grey hair, the pigmented follicles are usually the first to be affected leaving just white hair surviving in a patch of AA – although with time even white hair can be lost. As a result of this phenomena, some dermatologists believe that immunological action on hair follicles is specifically directed towards pigment producing melanocyte cells inside the hair follicles. Hair follicles with many active melanocytes, and making pigmented hair, may be easy targets for the immune cells to attack. Follicles with few melanocytes and/or inactive melanocytes, and producing gray hair, may be less stimulatory to the immune cells and so largely escape attack – for a while at least.
A rare form of AA called “alopecia areata nevi” gives rise to hair loss in the immediate area of moles or similar anomalous skin growths. The differences within these distinctive patches of skin somehow make hair follicles in the immediate area more sensitive to AA. If pigmentation does make hair follicles more susceptible then hair follicles in moles (as hyperpigmented areas of skin) may well be more susceptible to AA.
Skin Mosaicism: A hypothesis of “skin mosaicism” has been put forward to at least partially explain differences in hair follicles in different areas of the scalp. The cells that make up our skin are descendant from a very few embryonic cells and the skin can be divided into different regions depending on which embryonic cells multiplied to produce it. We know that the skin and hair of the scalp occipital region (the area that runs in a band from one ear around the back of the head to the other ear within the hair line) is derived from a different group of embryonic cells than the hair and skin on top of the head. Particularly intriguing is that “ophiasis” type alopecia areata is limited to hair loss in this occipital region, while hair follicles on the top and sides are not affected. Of course it is very tempting to speculate that this hair loss pattern is due in part to a subtle difference in the cells which gave rise to the occipital region of skin and hair follicles – although there is no direct evidence to prove this hypothesis.
Conclusion: The well-defined, but localized, pattern of hair loss in alopecia areata reflects a complex interplay of genetic, immunological, and environmental factors. The phenomenon of immune privilege collapse, coupled with the heterogeneity of hair follicles and the localized immune response, contributes to the selective targeting of hair follicles by the autoimmune process. Although significant progress has been made in understanding the mechanisms underlying AA, further research is necessary to fully elucidate why only certain hair follicles are affected. This knowledge will be important for developing targeted therapies that can protect hair follicles from autoimmune attacks or restore the immune privilege of affected follicles, offering hope for individuals suffering from this distressing condition.
Bibliography
11711645 {11711645:Q2X4UBMU},{11711645:PVKC22PJ},{11711645:XB2HSM3A},{11711645:6NJWJ5TQ},{11711645:8RH23T55},{11711645:G2TQEEGN},{11711645:M7FJF2PJ},{11711645:J8P34RKP},{11711645:WX26DGH5},{11711645:SZXNB4MQ},{11711645:FPAX6X2A},{11711645:VQG4IWRM},{11711645:HX5269VD},{11711645:CGCU43J2},{11711645:RC5BJJQ2},{11711645:8KQ43AVS},{11711645:K9JB6323} 1 vancouver 50 date asc 1160 https://www.keratin.com/wp-content/plugins/zotpress/ %7B%22status%22%3A%22success%22%2C%22updateneeded%22%3Afalse%2C%22instance%22%3Afalse%2C%22meta%22%3A%7B%22request_last%22%3A0%2C%22request_next%22%3A0%2C%22used_cache%22%3Atrue%7D%2C%22data%22%3A%5B%7B%22key%22%3A%228KQ43AVS%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Winkelmann%20and%20Jaffe%22%2C%22parsedDate%22%3A%221960-11%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BWinkelmann%20RK%2C%20Jaffe%20MO.%20Nerve%20network%20of%20the%20hair%20follicle%20in%20alopecia%20areata.%20Arch%20Dermatol.%201960%20Nov%3B82%3A750%26%23x2013%3B3.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Nerve%20network%20of%20the%20hair%20follicle%20in%20alopecia%20areata%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22R.%20K.%22%2C%22lastName%22%3A%22Winkelmann%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22M.%20O.%22%2C%22lastName%22%3A%22Jaffe%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%221960-11%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1001%5C%2Farchderm.1960.01580050092013%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%220003-987X%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AJQ7SV33%22%5D%2C%22dateModified%22%3A%222024-02-05T15%3A48%3A42Z%22%7D%7D%2C%7B%22key%22%3A%228RH23T55%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Eckert%20et%20al.%22%2C%22parsedDate%22%3A%221968-04%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BEckert%20J%2C%20Church%20RE%2C%20Ebling%20FJ.%20The%20pathogenesis%20of%20alopecia%20areata.%20Br%20J%20Dermatol.%201968%20Apr%3B80%284%29%3A203%26%23x2013%3B10.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22The%20pathogenesis%20of%20alopecia%20areata%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22J.%22%2C%22lastName%22%3A%22Eckert%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22R.%20E.%22%2C%22lastName%22%3A%22Church%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22F.%20J.%22%2C%22lastName%22%3A%22Ebling%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%221968-04%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1111%5C%2Fj.1365-2133.1968.tb11960.x%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%220007-0963%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AJQ7SV33%22%5D%2C%22dateModified%22%3A%222024-02-05T16%3A01%3A34Z%22%7D%7D%2C%7B%22key%22%3A%22J8P34RKP%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22H%5Cu00f6nemann%20and%20H%5Cu00f6fer%22%2C%22parsedDate%22%3A%221970-07%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BH%26%23xF6%3Bnemann%20W%2C%20H%26%23xF6%3Bfer%20W.%20%5BAre%20there%20any%20connections%20between%20sensory%20innervation%20of%20the%20head%20and%20location%20of%20the%20alopecia%20areata%20foci%3F%5D.%20Dermatol%20Monatsschr.%201970%20July%3B156%287%29%3A683%26%23x2013%3B90.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22%5BAre%20there%20any%20connections%20between%20sensory%20innervation%20of%20the%20head%20and%20location%20of%20the%20alopecia%20areata%20foci%3F%5D%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22W.%22%2C%22lastName%22%3A%22H%5Cu00f6nemann%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22W.%22%2C%22lastName%22%3A%22H%5Cu00f6fer%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%221970-07%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%22%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%220011-9083%22%2C%22language%22%3A%22ger%22%2C%22collections%22%3A%5B%22AJQ7SV33%22%5D%2C%22dateModified%22%3A%222024-02-05T15%3A47%3A41Z%22%7D%7D%2C%7B%22key%22%3A%22CGCU43J2%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Tobin%20et%20al.%22%2C%22parsedDate%22%3A%221990-06%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BTobin%20DJ%2C%20Fenton%20DA%2C%20Kendall%20MD.%20Ultrastructural%20observations%20on%20the%20hair%20bulb%20melanocytes%20and%20melanosomes%20in%20acute%20alopecia%20areata.%20J%20Invest%20Dermatol.%201990%20June%3B94%286%29%3A803%26%23x2013%3B7.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Ultrastructural%20observations%20on%20the%20hair%20bulb%20melanocytes%20and%20melanosomes%20in%20acute%20alopecia%20areata%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22D.%20J.%22%2C%22lastName%22%3A%22Tobin%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22D.%20A.%22%2C%22lastName%22%3A%22Fenton%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22M.%20D.%22%2C%22lastName%22%3A%22Kendall%22%7D%5D%2C%22abstractNote%22%3A%22It%20is%20well%20recognized%20that%20alopecia%20areata%20%28Aa%29%20may%20preferentially%20affect%20pigmented%20hair%20and%20may%20spare%20white%20hair%2C%20and%20that%20regrowing%20hair%20in%20the%20disease%20is%20often%20initially%20white.%20In%20addition%2C%20there%20is%20an%20association%20with%20vitiligo%20and%20ocular%20depigmentation.%20To%20date%2C%20the%20pathomechanisms%20of%20the%20melanocyte%20effects%20are%20unclear.%20We%20have%20studied%2010%20patients%20with%20untreated%20acute%20alopecia%20areata%2C%20and%20three%20normal%20patients%20without%20hair%20loss.%20Morphologic%20changes%2C%20studied%20by%20conventional%20light%20and%20electron%20microscopy%2C%20in%20the%20cytoplasm%20of%20affected%20melanocytes%20often%20predated%20nuclear%20hyperchromatism.%20Increased%20numbers%20of%20bizarre%20melanosomes%20were%20found%20in%20affected%20melanocytes%20compared%20with%20normal%20ones%3B%20such%20melanosomes%20had%20incomplete%20or%20%26quot%3Baborted%26quot%3B%20melanization%2C%20resulting%20in%20poor%20pigment%20deposition%2C%20and%20were%20disrupted%2C%20enlarged%20and%20rounded%2C%20with%20loss%20of%20normal%20ellipsoidal%20shape.%20An%20unusual%20outer%20root%20sheath%20%28ORS%29%20distribution%20of%20hair%20bulb%20melanocytes%20was%20seen.%20Other%20atypical%20melanosome%20effects%20included%20marked%20pigment%20displacement%20into%20peribulbar%20and%20DP%20melanophages.%20In%20the%20DP%20clumped%20melanin%20granules%20formed%20giant%20spherical%20complexes%20without%20discernible%20limiting%20membranes%2C%20which%20were%20sometimes%20associated%20with%20lymphocytes.%20These%20morphologic%20changes%20indicate%20an%20active%20involvement%20of%20hair%20bulb%20melanocytes%20in%20alopecia%20areata.%22%2C%22date%22%3A%221990-06%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1111%5C%2F1523-1747.ep12874660%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%220022-202X%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AJQ7SV33%22%5D%2C%22dateModified%22%3A%222024-02-05T16%3A19%3A59Z%22%7D%7D%2C%7B%22key%22%3A%22M7FJF2PJ%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Happle%22%2C%22parsedDate%22%3A%221993-11%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BHapple%20R.%20Mosaicism%20in%20human%20skin.%20Understanding%20the%20patterns%20and%20mechanisms.%20Arch%20Dermatol.%201993%20Nov%3B129%2811%29%3A1460%26%23x2013%3B70.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Mosaicism%20in%20human%20skin.%20Understanding%20the%20patterns%20and%20mechanisms%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22R.%22%2C%22lastName%22%3A%22Happle%22%7D%5D%2C%22abstractNote%22%3A%22BACKGROUND%3A%20The%20skin%20is%20especially%20suitable%20for%20the%20study%20of%20mosaicism.%20In%20this%20review%2C%20the%20various%20genetic%20mechanisms%20leading%20to%20mosaicism%20and%20the%20resulting%20cutaneous%20patterns%20are%20considered.%5CnOBSERVATIONS%3A%20Mosaicism%20may%20produce%20different%20cutaneous%20patterns%20such%20as%20the%20lines%20of%20Blaschko%2C%20the%20checkerboard%20pattern%2C%20the%20phylloid%20pattern%2C%20and%20a%20patchy%20pattern%20without%20midline%20separation.%20A%20unique%20lateralization%20pattern%20is%20observed%20in%20the%20CHILD%20syndrome.%20Two%20major%20genetic%20categories%20are%20functional%20mosaics%20resulting%20from%20X%20inactivation%20and%20genomic%20mosaics%20caused%20by%20autosomal%20mutations.%20Functional%20mosaicism%20may%20be%20caused%20by%20either%20male-lethal%20or%20nonlethal%20X-linked%20mutations.%20Similarly%2C%20autosomal%20mutations%20resulting%20in%20genomic%20mosaicism%20may%20be%20either%20lethal%20or%20nonlethal.%20Many%20mosaics%20are%20caused%20by%20loss%20of%20heterozygosity%2C%20and%20uncommonly%20this%20mechanism%20may%20give%20rise%20to%20twin%20spots%20such%20as%20vascular%20twin%20nevi.%20Some%20cutaneous%20mosaic%20phenotypes%20virtually%20always%20occur%20sporadically%2C%20but%20exceptionally%20may%20show%20a%20familial%20aggregation.%20This%20paradox%20may%20be%20explained%20by%20paradominant%20inheritance.%20Heterozygous%20individuals%20are%2C%20as%20a%20rule%2C%20unaffected%2C%20but%20they%20express%20the%20birthmark%20when%20allelic%20loss%20occurs%20during%20embryogenesis.%5CnCONCLUSIONS%3A%20The%20concept%20of%20cutaneous%20mosaicism%20is%20important%20for%20gene%20mapping%20because%20here%20we%20have%20the%20opportunity%20to%20study%20two%20populations%20of%20cells%20differing%20only%20with%20regard%20to%20the%20mutation%20causing%20mosaicism.%20Future%20research%20will%20probably%20show%20that%20a%20specific%20genetic%20anomaly%2C%20when%20present%20as%20a%20mosaic%2C%20always%20produces%20the%20same%20type%20of%20cutaneous%20pattern.%22%2C%22date%22%3A%221993-11%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%22%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%220003-987X%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AJQ7SV33%22%5D%2C%22dateModified%22%3A%222024-02-05T16%3A06%3A31Z%22%7D%7D%2C%7B%22key%22%3A%22K9JB6323%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Ziller%22%2C%22parsedDate%22%3A%221996%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BZiller%20C.%20Pattern%20formation%20in%20neural%20crest%20derivatives.%20In%3A%20Van%20Neste%20D%2C%20Randall%20V%2C%20editors.%20Hair%20Research%20for%20the%20Next%20Millennium.%20Amsterdam%3A%20Elsevier%3B%201996.%20p.%2019%26%23x2013%3B23.%20%28Excerpta%20Med%20Int%20Congr%3B%20vol.%201111%29.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22bookSection%22%2C%22title%22%3A%22Pattern%20formation%20in%20neural%20crest%20derivatives%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22C%22%2C%22lastName%22%3A%22Ziller%22%7D%2C%7B%22creatorType%22%3A%22editor%22%2C%22firstName%22%3A%22D%22%2C%22lastName%22%3A%22Van%20Neste%22%7D%2C%7B%22creatorType%22%3A%22editor%22%2C%22firstName%22%3A%22V%22%2C%22lastName%22%3A%22Randall%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22bookTitle%22%3A%22Hair%20Research%20for%20the%20Next%20Millennium%22%2C%22date%22%3A%221996%22%2C%22originalDate%22%3A%22%22%2C%22originalPublisher%22%3A%22%22%2C%22originalPlace%22%3A%22%22%2C%22format%22%3A%22%22%2C%22ISBN%22%3A%22%22%2C%22DOI%22%3A%22%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22ISSN%22%3A%22%22%2C%22language%22%3A%22%22%2C%22collections%22%3A%5B%22AJQ7SV33%22%5D%2C%22dateModified%22%3A%222024-02-05T16%3A11%3A55Z%22%7D%7D%2C%7B%22key%22%3A%22VQG4IWRM%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Rossi%20et%20al.%22%2C%22parsedDate%22%3A%221997-03-24%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BRossi%20R%2C%20Del%20Bianco%20E%2C%20Isolani%20D%2C%20Baccari%20MC%2C%20Cappugi%20P.%20Possible%20involvement%20of%20neuropeptidergic%20sensory%20nerves%20in%20alopecia%20areata.%20Neuroreport.%201997%20Mar%2024%3B8%285%29%3A1135%26%23x2013%3B8.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Possible%20involvement%20of%20neuropeptidergic%20sensory%20nerves%20in%20alopecia%20areata%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22R.%22%2C%22lastName%22%3A%22Rossi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22E.%22%2C%22lastName%22%3A%22Del%20Bianco%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22D.%22%2C%22lastName%22%3A%22Isolani%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22M.%20C.%22%2C%22lastName%22%3A%22Baccari%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22P.%22%2C%22lastName%22%3A%22Cappugi%22%7D%5D%2C%22abstractNote%22%3A%22Alopecia%20areata%20%28AA%29%20is%20a%20dermatosis%20involving%20the%20sudden%20occurrence%20of%20bald%20patches%20on%20the%20scalp.%20Although%20the%20aetiology%20is%20unknown%2C%20experimental%20data%20indicate%20that%20cutaneous%20microcirculation%20plays%20an%20important%20role.%20The%20skin%20is%20richly%20innervated%20by%20neuropeptidergic%20sensory%20nerves%20that%20help%20regulate%20microvascular%20circulation.%20This%20study%20shows%20a%20reduction%20of%20cutaneous%20levels%20of%20substance%20P%20and%20calcitonin%20gene-related%20peptide%20%28CGRP%29%20but%20not%20of%20vasoactive%20intestinal%20polypeptide%20in%20scalp%20biopsies%20from%20patients%20with%20AA.%20Laser-Doppler%20flowmetry%20was%20used%20to%20study%20microcirculation%20of%20the%20scalp.%20Results%20indicate%20that%20patients%20with%20AA%20have%20lower%20basal%20blood%20flow%20and%20greater%20vasodilatation%20following%20intradermal%20CGRP%20injection%20than%20control%20subjects.%20A%20vascular%20hyper-reactivity%20to%20vasodilatatory%20substances%20such%20as%20neuropeptides%2C%20probably%20because%20of%20the%20lack%20of%20these%20substances%2C%20is%20hypothesized.%22%2C%22date%22%3A%221997-03-24%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1097%5C%2F00001756-199703240-00015%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%220959-4965%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AJQ7SV33%22%5D%2C%22dateModified%22%3A%222024-02-05T15%3A48%3A08Z%22%7D%7D%2C%7B%22key%22%3A%22PVKC22PJ%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Botchkarev%22%2C%22parsedDate%22%3A%222003-10%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BBotchkarev%20VA.%20Neurotrophins%20and%20their%20role%20in%20pathogenesis%20of%20alopecia%20areata.%20J%20Investig%20Dermatol%20Symp%20Proc.%202003%20Oct%3B8%282%29%3A195%26%23x2013%3B8.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Neurotrophins%20and%20their%20role%20in%20pathogenesis%20of%20alopecia%20areata%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Vladimir%20A.%22%2C%22lastName%22%3A%22Botchkarev%22%7D%5D%2C%22abstractNote%22%3A%22Neurotrophins%20comprise%20a%20family%20of%20structurally%20and%20functionally%20related%20proteins%20that%20are%20critical%20for%20the%20development%20and%20maintenance%20of%20cutaneous%20innervation.%20They%20also%20fulfill%20multiple%20non-neurotrophic%20functions%20in%20skin%2C%20including%20regulation%20of%20epidermal%20proliferation%20and%20apoptosis%2C%20control%20of%20hair%20follicle%20development%20and%20cycling%2C%20and%20melanogenesis.%20Numerous%20indications%20suggest%20that%20neurotrophins%20play%20an%20important%20role%20in%20the%20pathogenesis%20of%20a%20variety%20of%20autoimmune%20diseases.%20In%20this%20review%2C%20we%20focus%20on%20the%20role%20of%20neurotrophins%20in%20the%20pathogenesis%20of%20alopecia%20areata%2C%20an%20autoimmune%20disorder%20that%20affects%20actively%20growing%20hair%20follicles.%20Recent%20data%20suggest%20that%20neurotrophins%20and%20their%20receptors%20are%20differentially%20expressed%20among%20the%20subsets%20of%20immune%20cells%20in%20alopecia%20areata-affected%20skin.%20Experimental%20data%20suggest%20that%20neurotrophins%20may%20regulate%20both%20the%20cyclic%20activity%20of%20the%20hair%20follicle%20and%20the%20functions%20of%20immune%20cells%20of%20inflammatory%20infiltrates.%20Additional%20research%20is%20required%20to%20bridge%20the%20gap%20between%20our%20current%20knowledge%20of%20neurotrophin%20functions%20in%20skin%20affected%20by%20alopecia%20areata%20and%20our%20knowledge%20of%20their%20potential%20clinical%20applications.%20Progress%20in%20this%20area%20of%20research%20will%20hopefully%20lead%20to%20the%20development%20of%20multiple%20applications%20for%20neurotrophins%20and%20their%20agonists%5C%2Fantagonists%20in%20alopecia%20areata%20and%20other%20hair%20growth%20disorders.%22%2C%22date%22%3A%222003-10%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1046%5C%2Fj.1087-0024.2003.00808.x%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221087-0024%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AJQ7SV33%22%5D%2C%22dateModified%22%3A%222024-02-05T15%3A47%3A27Z%22%7D%7D%2C%7B%22key%22%3A%22HX5269VD%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Siebenhaar%20et%20al.%22%2C%22parsedDate%22%3A%222007-06%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BSiebenhaar%20F%2C%20Sharov%20AA%2C%20Peters%20EMJ%2C%20Sharova%20TY%2C%20Syska%20W%2C%20Mardaryev%20AN%2C%20et%20al.%20Substance%20P%20as%20an%20immunomodulatory%20neuropeptide%20in%20a%20mouse%20model%20for%20autoimmune%20hair%20loss%20%28alopecia%20areata%29.%20J%20Invest%20Dermatol.%202007%20June%3B127%286%29%3A1489%26%23x2013%3B97.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Substance%20P%20as%20an%20immunomodulatory%20neuropeptide%20in%20a%20mouse%20model%20for%20autoimmune%20hair%20loss%20%28alopecia%20areata%29%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Frank%22%2C%22lastName%22%3A%22Siebenhaar%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Andrey%20A.%22%2C%22lastName%22%3A%22Sharov%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Eva%20M.%20J.%22%2C%22lastName%22%3A%22Peters%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Tatyana%20Y.%22%2C%22lastName%22%3A%22Sharova%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Wolfgang%22%2C%22lastName%22%3A%22Syska%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Andrei%20N.%22%2C%22lastName%22%3A%22Mardaryev%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Pia%22%2C%22lastName%22%3A%22Freyschmidt-Paul%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22John%20P.%22%2C%22lastName%22%3A%22Sundberg%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Marcus%22%2C%22lastName%22%3A%22Maurer%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Vladimir%20A.%22%2C%22lastName%22%3A%22Botchkarev%22%7D%5D%2C%22abstractNote%22%3A%22Alopecia%20areata%20%28AA%29%20is%20an%20autoimmune%20disorder%20of%20the%20hair%20follicle%20characterized%20by%20inflammatory%20cell%20infiltrates%20around%20actively%20growing%20%28anagen%29%20hair%20follicles.%20Substance%20P%20%28SP%29%20plays%20a%20critical%20role%20in%20the%20cutaneous%20neuroimmune%20network%20and%20influences%20immune%20cell%20functions%20through%20the%20neurokinin-1%20receptor%20%28NK-1R%29.%20To%20better%20understand%20the%20role%20of%20SP%20as%20an%20immunomodulatory%20neuropeptide%20in%20AA%2C%20we%20studied%20its%20expression%20and%20effects%20on%20immune%20cells%20in%20a%20C3H%5C%2FHeJ%20mouse%20model%20for%20AA.%20During%20early%20stages%20of%20AA%20development%2C%20the%20number%20of%20SP-immunoreactive%20nerve%20fibers%20in%20skin%20is%20increased%2C%20compared%20to%20non-affected%20mice.%20However%2C%20during%20advanced%20stages%20of%20AA%2C%20the%20number%20of%20SP-immunoreactive%20nerves%20and%20SP%20protein%20levels%20in%20skin%20are%20decreased%2C%20whereas%20the%20expression%20of%20the%20SP-degrading%20enzyme%20neutral%20endopeptidase%20%28NEP%29%20is%20increased%2C%20compared%20to%20control%20skin.%20In%20AA%2C%20NK-1R%20is%20expressed%20on%20CD8%2B%20lymphocytes%20and%20macrophages%20accumulating%20around%20affected%20hair%20follicles.%20Additional%20SP%20supply%20to%20the%20skin%20of%20AA-affected%20mice%20leads%20to%20a%20significant%20increase%20of%20mast%20cell%20degranulation%20and%20to%20accelerated%20hair%20follicle%20regression%20%28catagen%29%2C%20accompanied%20by%20an%20increase%20of%20CD8%2B%20cells-expressing%20granzyme%20B.%20These%20data%20suggest%20that%20SP%2C%20NEP%2C%20and%20NK-1R%20serve%20as%20important%20regulators%20in%20the%20molecular%20signaling%20network%20modulating%20inflammatory%20response%20in%20autoimmune%20hair%20loss.%22%2C%22date%22%3A%222007-06%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1038%5C%2Fsj.jid.5700704%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221523-1747%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AJQ7SV33%22%5D%2C%22dateModified%22%3A%222024-02-05T15%3A48%3A27Z%22%7D%7D%2C%7B%22key%22%3A%22XB2HSM3A%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22D%27Ovidio%22%2C%22parsedDate%22%3A%222013-04%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BD%26%23x2019%3BOvidio%20R.%20Koebner%20phenomenon%20in%20alopecia%20areata%3A%20rapid%20appearance%20after%20trichogram.%20Implications%20for%20the%20pathogenesis%20and%20therapy.%20G%20Ital%20Dermatol%20Venereol.%202013%20Apr%3B148%282%29%3A225%26%23x2013%3B9.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Koebner%20phenomenon%20in%20alopecia%20areata%3A%20rapid%20appearance%20after%20trichogram.%20Implications%20for%20the%20pathogenesis%20and%20therapy%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22R.%22%2C%22lastName%22%3A%22D%27Ovidio%22%7D%5D%2C%22abstractNote%22%3A%22Anecdotical%20experiences%20indicate%20that%20Koebner%20phenomenon%20%28KP%29%20can%20also%20be%20observed%20in%20alopecia%20areata%20%28AA%29.%20The%20present%20short%20report%20gives%20an%20account%20of%20what%20has%20been%20observed%20in%20some%20patients%20with%20remitting-relapsing%20AA%20in%20multiple%20patches%2C%20in%20whom%20the%20phenomenon%20was%20accidentally%20caused%20by%20perilesional%20Trichogram.%20The%20almost%20immediate%20appearance%20of%20relapses%20of%20the%20disease%20%281-7%20days%29%20and%20their%20evolution%20can%20be%20useful%20to%20understand%20the%20physiopathology%20of%20AA%20and%20and%20emphasize%20the%20compelling%20need%20for%20a%20rapid%20and%20appropriate%20diagnosis%20and%20treatment%20in%20the%20acute%20phase%20of%20AA%2C%20even%20with%20the%20active%20participation%20of%20the%20patient%20adequately%20trained.%20The%20method%20of%20trichogram%20should%20be%20reserved%20for%20cases%20in%20which%20non-invasive%20methods%20such%20as%20the%20Pull%20Test%20or%20Trichoscopy%20are%20not%20sufficient%20to%20verify%20the%20activity%20of%20the%20disease.%22%2C%22date%22%3A%222013-04%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%22%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%220392-0488%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AJQ7SV33%22%5D%2C%22dateModified%22%3A%222024-02-05T15%3A58%3A58Z%22%7D%7D%2C%7B%22key%22%3A%226NJWJ5TQ%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Delorenze%20et%20al.%22%2C%22parsedDate%22%3A%222016%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BDelorenze%20LM%2C%20Gavazzoni-Dias%20MFR%2C%20Teixeira%20MS%2C%20Aide%20MK.%20Concentric%20Polycyclic%20Regrowth%20Pattern%20in%20Alopecia%20Areata.%20Int%20J%20Trichology.%202016%3B8%281%29%3A35%26%23x2013%3B7.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Concentric%20Polycyclic%20Regrowth%20Pattern%20in%20Alopecia%20Areata%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Lilian%20Mathias%22%2C%22lastName%22%3A%22Delorenze%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Maria%20Fernanada%20Reis%22%2C%22lastName%22%3A%22Gavazzoni-Dias%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Marcelo%20S.%22%2C%22lastName%22%3A%22Teixeira%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Marcia%20Kalil%22%2C%22lastName%22%3A%22Aide%22%7D%5D%2C%22abstractNote%22%3A%22Alopecia%20areata%20%28AA%29%20is%20a%20common%20form%20of%20autoimmune%20nonscarring%20hair%20loss%20of%20scalp%20and%5C%2For%20body.%20Atypical%20hair%20regrowth%20in%20AA%20is%20considered%20a%20rare%20phenomenon.%20It%20includes%20atypical%20pattern%20of%20hair%20growth%20%28sudden%20graying%2C%20perinevoid%20alopecia%2C%20Renbok%20phenomenon%2C%20castling%20phenomenon%2C%20and%20concentric%20or%20targetoid%20regrowth%29%20and%20atypical%20dark%20color%20hair%20regrowth.%20We%20report%20a%20case%20of%20AA%20that%20resulted%20in%20a%20concentric%20targetoid%20hair%20regrowth%20and%20discuss%20the%20possible%20related%20theories%20regarding%20the%20significance%20of%20this%20phenomenon.%22%2C%22date%22%3A%222016%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.4103%5C%2F0974-7753.179397%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%220974-7753%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AJQ7SV33%22%5D%2C%22dateModified%22%3A%222024-02-05T16%3A00%3A01Z%22%7D%7D%2C%7B%22key%22%3A%22FPAX6X2A%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Li%20and%20Sinclair%22%2C%22parsedDate%22%3A%222016-02%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BLi%20J%2C%20Sinclair%20R.%20Clinical%20observations%20in%20alopecia%20areata%3A%20Implications%20and%20hypotheses.%20Australas%20J%20Dermatol.%202016%20Feb%3B57%281%29%3Ae29-31.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Clinical%20observations%20in%20alopecia%20areata%3A%20Implications%20and%20hypotheses%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Jane%22%2C%22lastName%22%3A%22Li%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Rod%22%2C%22lastName%22%3A%22Sinclair%22%7D%5D%2C%22abstractNote%22%3A%22Alopecia%20areata%20%28AA%29%20is%20a%20T-cell-mediated%20hair%20loss%20disorder%20but%20the%20exact%20cause%20is%20unknown.%20In%20this%20report%20we%20describe%20patterns%20of%20onset%2C%20regrowth%20and%20relapse%20in%20AA%20and%20propose%20potential%20underlying%20mechanisms.%20We%20believe%20that%20these%20aspects%20of%20AA%20require%20integration%20into%20modern%20theories%20of%20AA%20pathogenesis.%22%2C%22date%22%3A%222016-02%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1111%5C%2Fajd.12227%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221440-0960%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AJQ7SV33%22%5D%2C%22dateModified%22%3A%222024-02-05T15%3A57%3A49Z%22%7D%7D%2C%7B%22key%22%3A%22G2TQEEGN%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Farah%20et%20al.%22%2C%22parsedDate%22%3A%222016-12%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BFarah%20RS%2C%20Farah%20RS%2C%20Junqueira%20Bertin%20AC%2C%20Guo%20H%2C%20Ericson%20ME%2C%20Hordinsky%20MK.%20Increased%20cutaneous%20stimulation%20is%20required%20for%20C-fiber%20sensory%20perception%20in%20alopecia%20areata%3A%20A%20double-blind%20study.%20J%20Am%20Acad%20Dermatol.%202016%20Dec%3B75%286%29%3A1265%26%23x2013%3B7.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Increased%20cutaneous%20stimulation%20is%20required%20for%20C-fiber%20sensory%20perception%20in%20alopecia%20areata%3A%20A%20double-blind%20study%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ronda%20S.%22%2C%22lastName%22%3A%22Farah%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Rina%20S.%22%2C%22lastName%22%3A%22Farah%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Ana%20Carina%22%2C%22lastName%22%3A%22Junqueira%20Bertin%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Hongfei%22%2C%22lastName%22%3A%22Guo%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Marna%20E.%22%2C%22lastName%22%3A%22Ericson%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Maria%20K.%22%2C%22lastName%22%3A%22Hordinsky%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222016-12%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.jaad.2016.08.033%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221097-6787%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AJQ7SV33%22%5D%2C%22dateModified%22%3A%222024-02-05T15%3A47%3A54Z%22%7D%7D%2C%7B%22key%22%3A%22WX26DGH5%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Juhasz%20and%20Mesinkovska%22%2C%22parsedDate%22%3A%222019-08%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BJuhasz%20M%2C%20Mesinkovska%20NA.%20Are%20Preferred%20Scalp%20Locations%20for%20Alopecia%20Areata%20Patches%20a%20Clue%20to%20Neuronal%20Etiology%3F%20Skin%20Appendage%20Disord.%202019%20Aug%3B5%285%29%3A283%26%23x2013%3B7.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Are%20Preferred%20Scalp%20Locations%20for%20Alopecia%20Areata%20Patches%20a%20Clue%20to%20Neuronal%20Etiology%3F%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Margit%22%2C%22lastName%22%3A%22Juhasz%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Natasha%20Atanaskova%22%2C%22lastName%22%3A%22Mesinkovska%22%7D%5D%2C%22abstractNote%22%3A%22BACKGROUND%3A%20Alopecia%20areata%20%28AA%29%20is%20an%20autoimmune%20disease%20causing%20hair%20loss%20in%202%25%20of%20the%20population.%20Anecdotally%2C%20hair%20specialists%20report%20that%20patches%20localize%20to%20the%20scalp%20periphery.%20Changes%20in%20sensory%20innervation%20and%5C%2For%20scalp%20vasculature%20may%20play%20a%20role%20in%20the%20development%20and%20localization%20of%20alopecic%20patches.%5CnOBJECTIVE%3A%20To%20evaluate%20the%20most%20common%20locations%20of%20initial%20alopecic%20scalp%20patches.%5CnMATERIALS%20AND%20METHODS%3A%20A%20retrospective%20chart%20review%2C%20with%20comprehensive%20evaluation%20of%20clinical%20photographs%2C%20was%20conducted%20from%20July%202016%20to%20June%202018%20to%20include%20AA%20patients%20%28n%20%3D%20112%29.%20Clinical%20data%20was%20collected%20on%20gender%2C%20age%2C%20race%2C%20time%20until%20presentation%20at%20the%20clinic%2C%20and%20areas%20of%20hair%20loss%20on%20initial%20presentation.%5CnRESULTS%3A%20The%20most%20common%20areas%20of%20initial%20AA%20patches%20in%20both%20females%20and%20males%20were%20the%20occiput%20%2849%20vs.%2048.5%25%29%2C%20parietal%20%2846.9%20vs.%2021.2%25%29%2C%20vertex%20%2826.5%20vs.%2018.2%25%29%2C%20and%20frontal%20%2824.5%20vs.%2018.2%25%29%20regions%3B%2026.8%25%20of%20patients%20present%20with%20either%20alopecia%20totalis%20or%20universalis.%5CnLIMITATIONS%3A%20This%20is%20a%20single-center%20study%20with%20underrepresentation%20of%20minority%20races.%5CnCONCLUSION%3A%20AA%20patches%20most%20commonly%20present%20on%20the%20occiput%20of%20the%20scalp%20in%20both%20female%20and%20male%20patients.%20Cervical%20spine%20nerves%20C3%20and%20C2%20supply%20sensory%20innervation%20and%20the%20occipital%20artery%20supplies%20blood%20to%20this%20area.%22%2C%22date%22%3A%222019-08%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1159%5C%2F000497392%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%222296-9195%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AJQ7SV33%22%5D%2C%22dateModified%22%3A%222024-02-05T15%3A50%3A09Z%22%7D%7D%2C%7B%22key%22%3A%22RC5BJJQ2%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Watson%20et%20al.%22%2C%22parsedDate%22%3A%222022-06%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BWatson%20VE%2C%20Faniel%20ML%2C%20Kamili%20NA%2C%20Krueger%20LD%2C%20Zhu%20C.%20Immune-mediated%20alopecias%20and%20their%20mechanobiological%20aspects.%20Cells%20Dev.%202022%20June%3B170%3A203793.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Immune-mediated%20alopecias%20and%20their%20mechanobiological%20aspects%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Valencia%20E.%22%2C%22lastName%22%3A%22Watson%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Makala%20L.%22%2C%22lastName%22%3A%22Faniel%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Nourine%20A.%22%2C%22lastName%22%3A%22Kamili%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Loren%20D.%22%2C%22lastName%22%3A%22Krueger%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Cheng%22%2C%22lastName%22%3A%22Zhu%22%7D%5D%2C%22abstractNote%22%3A%22Alopecia%20is%20a%20non-specific%20term%20for%20hair%20loss%20clinically%20diagnosed%20by%20the%20hair%20loss%20pattern%20and%20histological%20analysis%20of%20patient%20scalp%20biopsies.%20The%20immune-mediated%20alopecia%20subtypes%2C%20including%20alopecia%20areata%2C%20lichen%20planopilaris%2C%20frontal%20fibrosing%20alopecia%2C%20and%20central%20centrifugal%20cicatricial%20alopecia%2C%20are%20common%2C%20significant%20forms%20of%20alopecia%20subtypes.%20For%20example%2C%20alopecia%20areata%20is%20the%20most%20common%20autoimmune%20disease%20with%20a%20lifetime%20incidence%20of%20approximately%202%25%20of%20the%20world%26%23039%3Bs%20population.%20In%20this%20perspective%2C%20we%20discuss%20major%20results%20from%20studies%20of%20immune-mediated%20alopecia%20subtypes.%20These%20studies%20suggest%20the%20key%20event%20in%20disease%20onset%20as%20the%20collapse%20in%20immune%20privilege%2C%20which%20alters%20the%20hair%20follicle%20microenvironment%2C%20e.g.%2C%20upregulation%20of%20major%20histocompatibility%20complex%20molecules%20and%20increase%20of%20cytokine%20production%2C%20and%20results%20in%20immune%20cell%20infiltration%2C%20inflammatory%20responses%2C%20and%20damage%20of%20hair%20follicles.%20We%20note%20that%20previous%20studies%20have%20established%20that%20the%20hair%20follicle%20has%20a%20complex%20mechanical%20microenvironment%2C%20which%20may%20regulate%20the%20function%20of%20not%20only%20tissue%20cells%20but%20also%20immune%20cell%20infiltrates.%20This%20suggests%20a%20potential%20for%20mechanobiology%20to%20contribute%20to%20alopecia%20research%20by%20adding%20new%20methods%2C%20new%20approaches%2C%20and%20new%20ways%20of%20thinking%2C%20which%20is%20missing%20in%20the%20existing%20literature.%20To%20fill%20this%20a%20gap%20in%20the%20alopecia%20research%20space%2C%20we%20develop%20a%20mechanobiological%20hypothesis%20that%20alterations%20in%20the%20hair%20follicle%20microenvironment%2C%20specifically%20in%20the%20mechanically%20responsive%20tissues%20and%20cells%2C%20partially%20due%20to%20loss%20of%20immune%20privilege%2C%20may%20be%20contributors%20to%20disease%20pathology.%20We%20further%20focus%20our%20discussion%20on%20the%20potential%20for%20applying%20mechanoimmunology%20to%20the%20study%20of%20T%20cell%20infiltrates%20in%20the%20hair%20follicle%2C%20as%20they%20are%20considered%20primary%20contributors%20to%20alopecia%20pathology.%20To%20establish%20the%20connection%20between%20the%20mechanoimmunological%20hypothesis%20and%20immune-mediated%20alopecia%20subtypes%2C%20we%20discuss%20what%20is%20known%20about%20the%20role%20of%20T%20cells%20in%20immune-mediated%20alopecia%20subtypes%2C%20using%20the%20most%20extensively%20studied%20AA%20as%20our%20model.%22%2C%22date%22%3A%222022-06%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.cdev.2022.203793%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%222667-2901%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AJQ7SV33%22%5D%2C%22dateModified%22%3A%222024-02-05T15%3A49%3A05Z%22%7D%7D%2C%7B%22key%22%3A%22SZXNB4MQ%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Lee%20and%20Lee%22%2C%22parsedDate%22%3A%222023-06%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BLee%20YB%2C%20Lee%20WS.%20Topographical%20Difference%20in%20the%20Prognosis%20of%20Alopecia%20Areata.%20Ann%20Dermatol.%202023%20June%3B35%283%29%3A240%26%23x2013%3B2.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22Topographical%20Difference%20in%20the%20Prognosis%20of%20Alopecia%20Areata%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Young%20Bin%22%2C%22lastName%22%3A%22Lee%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Won-Soo%22%2C%22lastName%22%3A%22Lee%22%7D%5D%2C%22abstractNote%22%3A%22%22%2C%22date%22%3A%222023-06%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.5021%5C%2Fad.20.329%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%222005-3894%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AJQ7SV33%22%5D%2C%22dateModified%22%3A%222024-02-05T15%3A49%3A53Z%22%7D%7D%2C%7B%22key%22%3A%22Q2X4UBMU%22%2C%22library%22%3A%7B%22id%22%3A11711645%7D%2C%22meta%22%3A%7B%22creatorSummary%22%3A%22Asz-Sigall%20et%20al.%22%2C%22parsedDate%22%3A%222023-10%22%2C%22numChildren%22%3A0%7D%2C%22bib%22%3A%22%26lt%3Bdiv%20class%3D%26quot%3Bcsl-bib-body%26quot%3B%20style%3D%26quot%3Bline-height%3A%201.35%3B%20%26quot%3B%26gt%3B%5Cn%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-entry%26quot%3B%20style%3D%26quot%3Bclear%3A%20left%3B%20%26quot%3B%26gt%3B%5Cn%20%20%20%20%26lt%3Bdiv%20class%3D%26quot%3Bcsl-left-margin%26quot%3B%20style%3D%26quot%3Bfloat%3A%20left%3B%20padding-right%3A%200.5em%3B%20text-align%3A%20right%3B%20width%3A%201em%3B%26quot%3B%26gt%3B1.%26lt%3B%5C%2Fdiv%26gt%3B%26lt%3Bdiv%20class%3D%26quot%3Bcsl-right-inline%26quot%3B%20style%3D%26quot%3Bmargin%3A%200%20.4em%200%201.5em%3B%26quot%3B%26gt%3BAsz-Sigall%20D%2C%20Ortega-Springall%20MF%2C%20Smith-Pliego%20M%2C%20Rodr%26%23xED%3Bguez-Lobato%20E%2C%20Martinez-Velasco%20MA%2C%20Arenas%20R%2C%20et%20al.%20White%20hair%20in%20alopecia%20areata%3A%20Clinical%20forms%20and%20proposed%20physiopathologic%20mechanisms.%20J%20Am%20Acad%20Dermatol.%202023%20Oct%3B89%284%29%3A758%26%23x2013%3B63.%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%20%20%20%26lt%3B%5C%2Fdiv%26gt%3B%5Cn%26lt%3B%5C%2Fdiv%26gt%3B%22%2C%22data%22%3A%7B%22itemType%22%3A%22journalArticle%22%2C%22title%22%3A%22White%20hair%20in%20alopecia%20areata%3A%20Clinical%20forms%20and%20proposed%20physiopathologic%20mechanisms%22%2C%22creators%22%3A%5B%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Daniel%22%2C%22lastName%22%3A%22Asz-Sigall%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mar%5Cu00eda%20Fernanda%22%2C%22lastName%22%3A%22Ortega-Springall%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Mariam%22%2C%22lastName%22%3A%22Smith-Pliego%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Erika%22%2C%22lastName%22%3A%22Rodr%5Cu00edguez-Lobato%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Maria%20Abril%22%2C%22lastName%22%3A%22Martinez-Velasco%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Roberto%22%2C%22lastName%22%3A%22Arenas%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Colombina%22%2C%22lastName%22%3A%22Vincenzi%22%7D%2C%7B%22creatorType%22%3A%22author%22%2C%22firstName%22%3A%22Antonella%22%2C%22lastName%22%3A%22Tosti%22%7D%5D%2C%22abstractNote%22%3A%22Alopecia%20areata%20%28AA%29%20is%20a%20common%20form%20of%20nonscarring%20hair%20loss.%20It%20is%20believed%20to%20be%20a%20consequence%20of%20an%20immune-mediated%20stimulus%2C%20probably%20involving%20autoreactive%20T%20cells%20against%20antigens%20present%20in%20the%20hair%20follicle.%20The%20exact%20antigen%20is%20still%20unknown%3B%20however%2C%20some%20authors%20have%20proposed%20that%20melanogenesis-associated%20molecules%20might%20trigger%20autoimmunity.%20Although%20transient%20white%20hair%20regrowth%20is%20a%20common%20and%20well-known%20situation%20in%20AA%2C%20there%20are%20other%20types%20of%20white%20hair%20phenomena%20in%20this%20context%2C%20including%20permanent%20white%20hair%20regrowth%2C%20sparing%20of%20white%20hair%20in%20a%20patchy%20pattern%2C%20or%20sparing%20in%20a%20diffuse%20pattern%2C%20giving%20the%20appearance%20of%20the%20so-called%20overnight%20graying%20phenomena%20or%20canitis%20subita.%20In%20this%20review%2C%20we%5Cu00a0aim%20to%20describe%20the%20different%20clinical%20aspects%20of%20white%20hair%20in%20AA%2C%20as%20well%20as%20the%20proposed%20pathophysiologic%20mechanisms%20involved%20in%20this%20phenomena.%22%2C%22date%22%3A%222023-10%22%2C%22section%22%3A%22%22%2C%22partNumber%22%3A%22%22%2C%22partTitle%22%3A%22%22%2C%22DOI%22%3A%2210.1016%5C%2Fj.jaad.2018.12.047%22%2C%22citationKey%22%3A%22%22%2C%22url%22%3A%22%22%2C%22PMID%22%3A%22%22%2C%22PMCID%22%3A%22%22%2C%22ISSN%22%3A%221097-6787%22%2C%22language%22%3A%22eng%22%2C%22collections%22%3A%5B%22AJQ7SV33%22%5D%2C%22dateModified%22%3A%222024-02-05T16%3A19%3A21Z%22%7D%7D%5D%7D 1.
Winkelmann RK, Jaffe MO. Nerve network of the hair follicle in alopecia areata. Arch Dermatol. 1960 Nov;82:750–3.
1.
Eckert J, Church RE, Ebling FJ. The pathogenesis of alopecia areata. Br J Dermatol. 1968 Apr;80(4):203–10.
1.
Hönemann W, Höfer W. [Are there any connections between sensory innervation of the head and location of the alopecia areata foci?]. Dermatol Monatsschr. 1970 July;156(7):683–90.
1.
Tobin DJ, Fenton DA, Kendall MD. Ultrastructural observations on the hair bulb melanocytes and melanosomes in acute alopecia areata. J Invest Dermatol. 1990 June;94(6):803–7.
1.
Happle R. Mosaicism in human skin. Understanding the patterns and mechanisms. Arch Dermatol. 1993 Nov;129(11):1460–70.
1.
Ziller C. Pattern formation in neural crest derivatives. In: Van Neste D, Randall V, editors. Hair Research for the Next Millennium. Amsterdam: Elsevier; 1996. p. 19–23. (Excerpta Med Int Congr; vol. 1111).
1.
Rossi R, Del Bianco E, Isolani D, Baccari MC, Cappugi P. Possible involvement of neuropeptidergic sensory nerves in alopecia areata. Neuroreport. 1997 Mar 24;8(5):1135–8.
1.
Botchkarev VA. Neurotrophins and their role in pathogenesis of alopecia areata. J Investig Dermatol Symp Proc. 2003 Oct;8(2):195–8.
1.
Siebenhaar F, Sharov AA, Peters EMJ, Sharova TY, Syska W, Mardaryev AN, et al. Substance P as an immunomodulatory neuropeptide in a mouse model for autoimmune hair loss (alopecia areata). J Invest Dermatol. 2007 June;127(6):1489–97.
1.
D’Ovidio R. Koebner phenomenon in alopecia areata: rapid appearance after trichogram. Implications for the pathogenesis and therapy. G Ital Dermatol Venereol. 2013 Apr;148(2):225–9.
1.
Delorenze LM, Gavazzoni-Dias MFR, Teixeira MS, Aide MK. Concentric Polycyclic Regrowth Pattern in Alopecia Areata. Int J Trichology. 2016;8(1):35–7.
1.
Li J, Sinclair R. Clinical observations in alopecia areata: Implications and hypotheses. Australas J Dermatol. 2016 Feb;57(1):e29-31.
1.
Farah RS, Farah RS, Junqueira Bertin AC, Guo H, Ericson ME, Hordinsky MK. Increased cutaneous stimulation is required for C-fiber sensory perception in alopecia areata: A double-blind study. J Am Acad Dermatol. 2016 Dec;75(6):1265–7.
1.
Juhasz M, Mesinkovska NA. Are Preferred Scalp Locations for Alopecia Areata Patches a Clue to Neuronal Etiology? Skin Appendage Disord. 2019 Aug;5(5):283–7.
1.
Watson VE, Faniel ML, Kamili NA, Krueger LD, Zhu C. Immune-mediated alopecias and their mechanobiological aspects. Cells Dev. 2022 June;170:203793.
1.
Lee YB, Lee WS. Topographical Difference in the Prognosis of Alopecia Areata. Ann Dermatol. 2023 June;35(3):240–2.
1.
Asz-Sigall D, Ortega-Springall MF, Smith-Pliego M, Rodríguez-Lobato E, Martinez-Velasco MA, Arenas R, et al. White hair in alopecia areata: Clinical forms and proposed physiopathologic mechanisms. J Am Acad Dermatol. 2023 Oct;89(4):758–63.